Clinical and Radiologic Findings
Recurrent aspiration of gastric contents, or chronic occult aspiration, is a common, often silent, process that especially affects infants with feeding problems, adults with neurologic deficits, and patients with decreased gastroesophageal motility and acid reflux. Recurrent aspiration is known to cause lung disease and recurrent pneumonia and may also be a contributing factor in exacerbating chronic lung diseases, such as idiopathic pulmonary fibrosis (IPF), chronic obstructive lung disease, chronic rejection in lung transplant patients, and cystic fibrosis.
In a series of patients with lung infiltrates and pulmonary symptoms that could not be explained by routine evaluation, almost half showed pulmonary aspiration by overnight scintigraphy, which correlated positively with obstructive sleep apnea and recurrent pneumonias.
1Gastroesophageal reflux disease (GERD) is a proven risk factor for recurrent microaspiration, which may cause lung injury. Unfortunately, there are no reliable widely used diagnostic tests for microaspiration. Proximal esophageal acid detection by pH monitoring is widely available but lacks sensitivity. Impedance monitoring measures both acid and nonacid reflux episodes and is therefore more sensitive.
2 In fact, experimental studies have shown that microaspiration is a fairly common phenomenon and can be seen in up to 40% of normal individuals and in up to 70% of people with neurologic alterations or obstructive sleep apnea. However, normal people tend to clear such aspirations without sequelae.
3,4 Aspiration pneumonia generally results from a single large event and is a common autopsy finding in debilitated patients with neurologic defects or other predisposing factors.
Common presenting symptoms of aspiration-induced lung disease include dyspnea, fever, and cough. There is a history of recurrent pneumonia in about 25% of patients. In addition to reflux and neurologic disease, drug use is an additional predisposing factor.
5 The most common clinical settings for aspiration are presented in
Table 25.1.
Chest radiograph shows bilateral infiltrates or nodules in about half, with unilateral findings in the other half. Areas most prone to aspiration are the right middle and lower lobes, due to the anatomic configuration of the bronchi. However, these vary depending on the patient’s position at the time of aspiration (e.g., sleep patterns). In some cases, nodules may be solitary and raise a clinical concern for malignancy. Computed tomography (CT) in patients with prominent small airway involvement typically shows centrilobular nodules in dependent portions of the lung. In aspiration pneumonia, imaging often demonstrates airspace disease (ground glass or consolidation), reticular densities, and nodules.
Gross and Histologic Findings
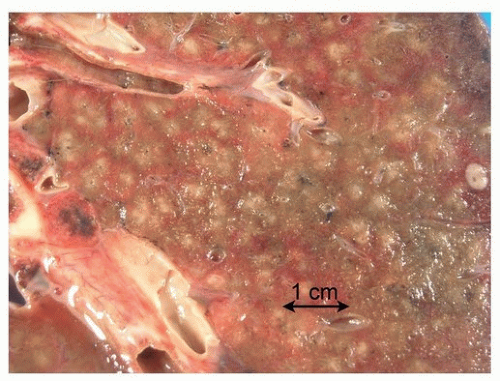
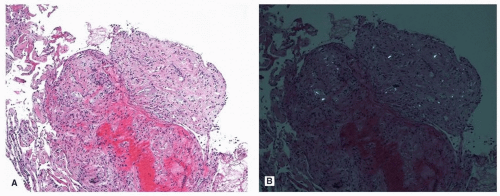
Aspiration pneumonia is characterized by patchy areas of consolidation (
Fig. 25.1). Abscess formation is not uncommon.
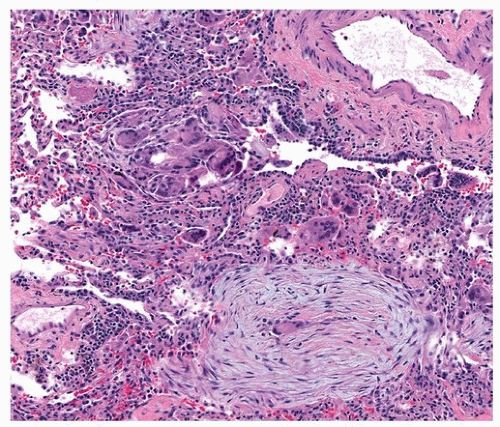
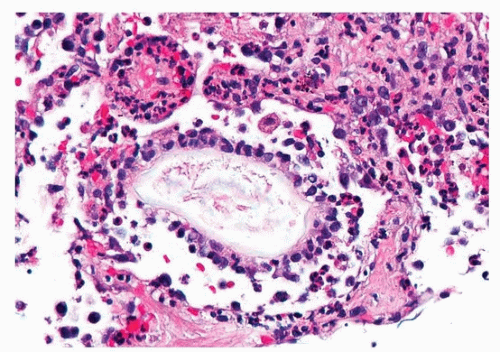
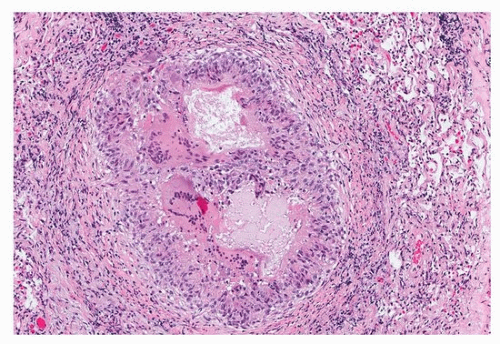
The histologic findings of aspiration depend on the type and amount of aspirated material. Aspiration of a large bolus of acid gastric content causes diffuse alveolar damage (Chapter 4). Aspiration of recurrent small amount of food or pills usually causes acute and organizing pneumonia with multinucleated foreign body giant cell reaction and suppurative granulomas. Chronic bronchiolitis may be the predominant histologic finding secondary to chronic occult aspiration.
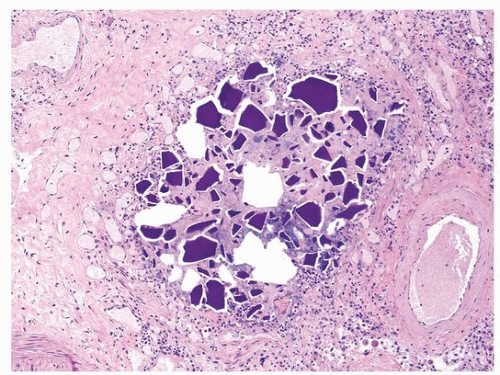
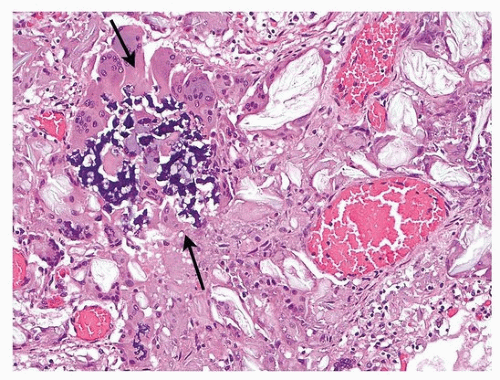
9 A definitive diagnosis rests on the identification of foreign material within the giant cells or suppurative granulomas (
Figs. 25.2,
25.3,
25.4).
5 The most common vegetable matter seen in chronic aspiration is the starch grain or granule, found in legumes, including peas, beans, and lentils. The starch granule is about 100 µ in length (
Fig. 25.3), is eosinophilic and well demarcated and oval, and eventually degenerates as macrophages engulf the material (
Fig. 25.4). Other foreign materials that may be seen in aspiration include cellulose (
Fig. 25.5), crospovidone (
Fig. 25.6), Kayexalate (
Fig. 25.7),
10 and talc (
Fig. 25.8), each with characteristic histologic features. If foreign material is not present,
a histologic diagnosis of aspiration pneumonia cannot be made, although can be surmised with clinical documentation of aspiration and exclusion of other causes of lung disease.
11Aspiration pneumonia may result in an infectious process due to superinfection by bacteria from the oropharynx or bacteria found in aspirated matter. Histologically, the features are those of an acute bronchopneumonia, often necrotizing, and foreign material may or may not be present.
11