Figure 26.1
(a–c) Classic CT scan appearance of aspergilloma in axial, sagittal, and coronal sections. Note the surrounding inflammation that is present in complex aspergilloma. As is typical, the fungal ball does not fill the cavitary space and is mobile within it. This air space leads to the radiologic crescent sign. (d–f), Upright, right lateral decubitus, and left lateral decubitus films demonstrate dependent movement of the ball within the cavity
Medical Therapy
Itraconazole is the medical therapy of choice, demonstrating some ability to penetrate the cavity. However, efficacy of medical therapy alone is poor (Walsh et al. 2008).
Surgical Indications
Surgical resection is the only chance for permanent cure of aspergilloma (Jewkes et al. 1983). However, due to the historically high morbidity of aspergilloma surgery, there remains controversy over the treatment of asymptomatic patients. We feel that our experience and the literature support resection of simple aspergilloma even when asymptomatic. It is known that hemoptysis occurs in up to 83 % of patients with aspergilloma (Karas et al. 1976) and the mortality rate of patients with hemoptysis is reported to be in the realm of 30 % (Uflacker et al. 1983). Additionally, resections of more advanced disease are more challenging and risky. All of these factors argue for early intervention, even when asymptomatic in appropriate patients. Those with severely compromised lung function may not be candidates for resection and this issue is addressed in Fig. 26.2.
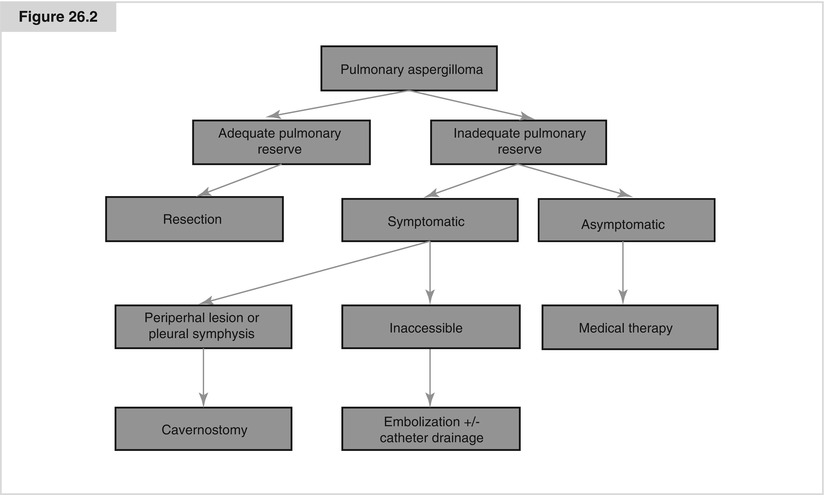
Figure 26.2
Algorithm to determine optimal therapy. Surgery is the only definitive therapy for aspergilloma. Those that are operative candidates should undergo resection of the cavity. Those that have inadequate pulmonary reserve and are asymptomatic should be observed until they develop symptoms. Those that are symptomatic can undergo non-resectional therapy for aspergilloma. In most cases, lesions are peripheral in the upper lobes and pleural symphysis is present. In these cases, mycetoma removal and cavity drainage can be accomplished by cavernostomy. However, when these conditions are not present, one may have to rely upon bronchial artery embolization and/or catheter based drainage of the cavity as the best therapy
Surgical Therapy
Surgery for aspergilloma is classically known to be challenging due to technical factors such as pleural adhesions and inflammatory changes in the hilum as well as patient factors such as comorbid conditions, poor lung function, and previous thoracic operations. Since the first report of resection of pulmonary aspergilloma in 1947 (Garvey et al. 1977), multiple case series have been published. It became well recognized that this operation carried a hefty mortality, as high as 23 % in a series by Daly and colleagues (1986). As one might expect, intraoperative blood loss is high with an average of 750 mL. Respiratory failure is the most common cause of death in the peri-operative period; thus making careful preoperative pulmonary function assessment critical in operative planning (Chen et al. 1997). Other complications contribute to high mortality and morbidity rates such as bronchopleural fistula and residual space with empyema. Those with advanced disease (complex aspergilloma) clearly have higher complications rates compared to early, simple aspergilloma, supporting the principle of early therapy (Henderson et al. 1975).
More recent reports, however, suggest that the results from resection of pulmonary aspergilloma may have improved over the years, though the morbidity and mortality rates remain high as compared to other thoracic procedures. Lejay recently reviewed 33 cases performed between 1998 and 2009 of surgical therapy for pulmonary aspergilloma. All underwent resection except for 2 with inadequate lung function undergoing cavernostomy. As compared to historic cohorts, the incidence of underlying tuberculosis had decreased from 57 to 15 %. Also the incidence of complex disease had decreased from 80 to 12 %. These two points suggest decreasing levels of complexity of cases over the past three decades likely due to the lower incidence of underlying tuberculosis. Mortality rate was 0 % in the modern series and morbidity rates had gone down significantly as well; major bleeding 44–6 %, pleural space problems 47–12 %, and prolonged hospitalization 32–6 % (Lejay et al 2011).
Notwithstanding these improved results in modern times, the comorbidities of many patients with aspergilloma as well as the technical difficulties involved with the operation dictate that a subgroup of patients may be better suited to a minimalistic approach known as cavernostomy.
Formal Resection
Aspergilloma is located in the upper lobes in 90 % of cases. The right upper lobe is the most commonly involved. Unilateral lung destruction is the rare indication for pneumonectomy (el Oakley et al. 1997). Bilateral disease can occasionally be treated with a staged operation. Resection is the treatment of choice for a fit patient, as more current evidence suggests reasonable morbidity and mortality with high cure rates from this therapy. Chen and coworkers reported a retrospective series with 67 patients with most undergoing lobectomy. Tuberculosis was the underlying cause in 80 % of cases. They reported a 25 % complication rate with one death in the only patient undergoing cavernostomy (Chen et al. 1997). Brik reported a series of 42 complex and simple aspergillomas. Five year survival was 93 % in the simple group and 83 % in the complex group. Patients required lobectomy in 86 % of cases and pneumonectomy in only 5 % (Brik et al. 2008).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


