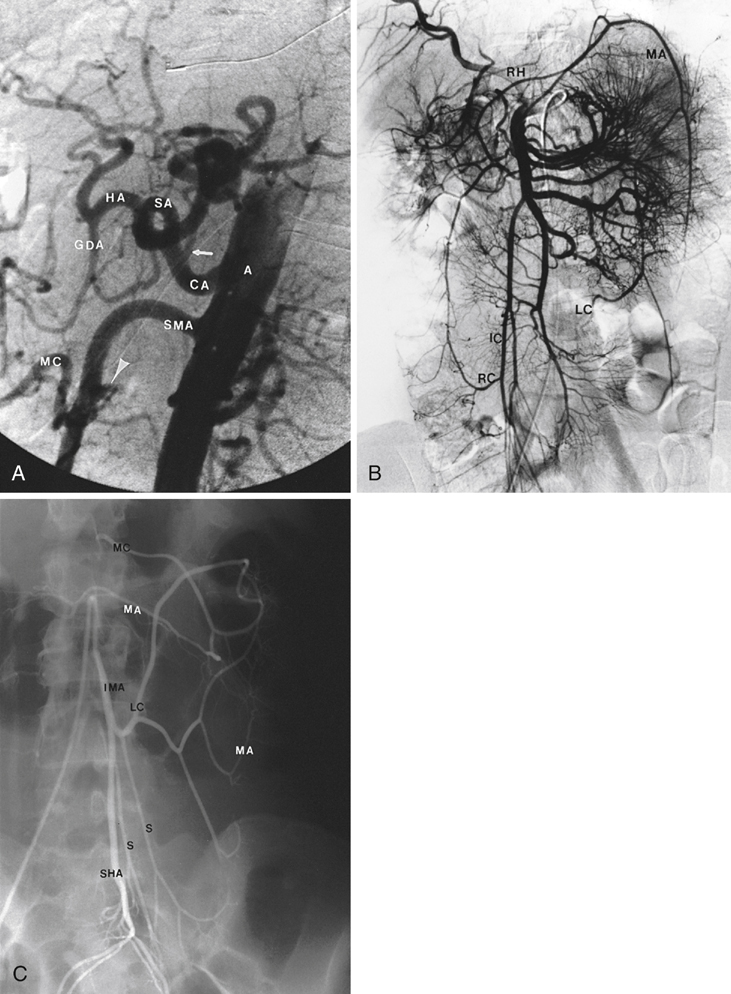
The celiac trunk, also called the celiac axis, arises from the ventral surface of the aorta below the aortic hiatus of the diaphragm between the T12 and L1 vertebral bodies. It supplies blood to the supper abdominal viscera (including the stomach, duodenum, spleen, pancreas, omentum, liver, diaphragm, and distal esophagus). The first portion of the celiac trunk, the celiac artery descends caudally for 1 to 2 cm and then curves ventrocaudally or ventrocranially (Figure 1A). It gives off the left gastric artery and then divides into the splenic and common hepatic arteries. The superior mesenteric artery arises from the ventral surface of the aorta approximately 1 to 2 cm below the origin of the celiac axis at the level of the disc space of the first and second lumbar vertebral bodies (see Figure 1A). Rarely the SMA arises from the celiac axis as a celiacomesenteric trunk or caudal to the origins of the renal arteries. The proximal part of the SMA courses behind the body of the pancreas in close proximity to the uncinate process in a 45- to 60-degree angle to the aorta. This angle may be more severe in patients with chronic mesenteric ischemia, making transfemoral stenting of SMA stenosis difficult. It ranges 8 to 10 mm in width at angiography. It supplies the duodenum, the pancreas, the small intestine, the cecum, and the ascending and transverse parts of the colon. The branches of the SMA are the inferior pancreaticoduodenal, middle colic, jejunal, ileal, right colic, and ileocolic arteries, respectively (see Figure 1B). The first branch of the SMA usually is the inferior pancreaticoduodenal (IPD) artery, which arises from the SMA or from the proximal jejunal branch. The anterior and posterior branches of the IPD ascend and anastomose with the anterior and posterior branches of the gastroduodenal artery. The jejunal (2–7) and ileal (7–17) branches arise from the left side of the SMA. These arteries form multiple mesenteric arcades, which increase in number distally. The vasa recta from the terminal arcades enter the bowel wall without intercommunication. The IMA arises from the left ventral surface of the abdominal aorta, usually at the level of the third lumbar vertebra. It courses caudally for 3 to 4 cm before giving off the left colic artery (see Figure 1C). The left colic artery gives rise to the marginal artery and one or more sigmoidal arteries. The branches of the left colic and sigmoidal arteries participate in the marginal artery of Drummond in the mesocolon. After giving off the left colic and sigmoidal branches, the IMA terminates as the superior rectal (superior hemorrhoidal) artery, which communicates with the middle rectal artery arising from the left internal iliac artery.
Arteriography Evaluation of Splanchnic Artery Occlusive Disease
Vascular Anatomy
Celiac Artery
Superior Mesenteric Artery
Inferior Mesenteric Artery
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


