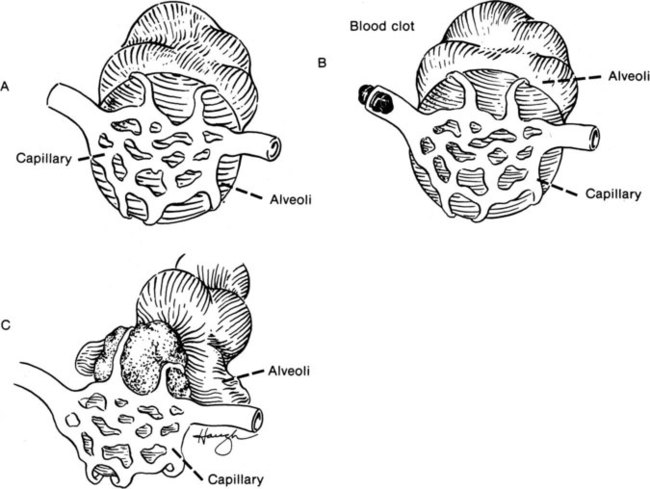
An arterial blood gas is a physiological assessment tool that measures a patient’s acid-base balance, alveolar ventilation, and oxygenation status.1 It is a valuable resource for obtaining information from respiratory monitoring in the intensive care unit, for conducting follow-up of outpatients, and for evaluating the treatment and the progress of their diseases. There has been a trend toward finding more noninvasive techniques to serve these purposes. This trend has been motivated by the desire to spare patients from being “stuck” so frequently and to avoid the risk for infection posed by indwelling cannulas in patients who already are ill and have weakened immune systems. Physical therapists frequently use oxygen saturation for assessment, but this is insufficient in many patients. When a patient has been thoroughly examined and it is determined that the arterial blood gas values are relatively stable, the physical therapist should compare those values to subsequent readings on the oximeter. Therapists need to consider the blood gas trends, acid/base status, and alveolar ventilation and then correlate those findings to the patient’s signs and symptoms, the physiological monitoring of HR, BP, and RR, and the perceived exertion with exercise. In many cases we need to consider a multisystem approach without examination and evaluation. Oximetry readings are important but must be evaluated in light of all body systems, not just the oximetry readings. Noninvasive monitoring has become more readily available and is used to measure expired carbon dioxide (Pet CO2) and transcutaneous CO2 (T CO2) in neonatal and pediatric patients. New studies are showing that a universal pulse oximetry screening of all neonates before they are discharged would improve the detection rate of congenital heart disease. In a survey conducted in the United Kingdom by Kang and colleagues, it was found that 209 (93%) of the 224 units contacted did not use pulse oximetry routinely. In the neonatal units that did use pulse oximetry, if the saturation was abnormal, they also did echocardiography. Two other units obtained not only echocardiogram, but also x-rays and ECG. The conclusion was that this should be used with national guidelines to supplement the postnatal examination.2 A similar study was conducted by Arlettaz and colleagues to determine whether pulse oximetry could detect congenital heart disease in newborns. It was noted that about half of all newborns who had congenital heart disease were asymptomatic in the first few days of their life. However, early detection of this condition is important because treatment outcomes are related to the time of the diagnosis, and early identification leads to best outcomes. The authors studied the effectiveness of oximetry on the first day of life for early detection of congenital heart disease in neonates who appeared normal. They also examined whether pulse oximeter screening in addition to the clinical examination of the patient would yield more results in the diagnosis of congenital heart disease than would examination alone. If pulse oximetry was less than 95%, echocardiography was done. Of the 3262 newborns screened, 24 infants had repeated oxygen saturations of less than 95%. Of these neonates, 17 had congenital heart disease and the other 5 had persistent pulmonary hypertension. Arlettaz and colleagues concluded that pulse oximetry screening in the first few days of life is an effective tool to identify cyanotic congenital heart disease in otherwise healthy newborns.3 Normally, alveolar units ventilate and capillary units bring oxygenated blood to the tissues, excreting CO2 back into the alveoli to be removed through the lungs. Some abnormal situations may occur, however, such as shunts and dead-space units. In a shunt unit, the alveoli have collapsed, but blood flow continues and is unable to pick up oxygen. An example of this is atelectasis, in which a lung segment or part of a segment has retained secretions and lung tissue distal to the mucous plug collapses. Circulation continues but oxygenation does not occur, and the PO2 decreases. On the other hand, a dead-space unit can have ventilation but not perfusion. This occurs with pulmonary embolism, when a blood clot obstructs the circulation. The oxygen is available in the ventilated alveoli, but with no circulation, a dead unit is credited. Figure 10-1 demonstrates the regional differences seen in respiratory units. Arterial oxygen is measured as PO2, the partial pressure of oxygen. Normal values are 80 to 100 mm Hg. If the PO2 is below 80 mm Hg in someone younger than 60 years of age, the patient is hypoxemic. A value of 60 to 80 mm Hg is considered mild hypoxemia; 40 to 60 mm Hg is considered moderate hypoxemia, and less than 40 mm Hg is severe hypoxemia.1
Arterial Blood Gases
Noninvasive Monitoring
Partial Pressure of Gases
Normal Blood Gas Values
Arterial Blood Gases