Arrhythmia
Bryan J. Baranowski
QUESTIONS
1.Which of the following antiarrhythmic medications would be the best choice for treatment of a patient with atrial fibrillation (AFib) and significant renal insufficiency?
a.Propafenone
b.Sotalol
c.Dofetilide
d.Flecainide
2.Which of the following antiarrhythmic medications has active metabolites?
a.Amiodarone
b.Sotalol
c.Dofetilide
d.Flecainide
3.A patient arrives at the emergency department with symptomatic narrow complex tachycardia. The patient is hemodynamically stable. The decision is made to administer intravenous (IV) adenosine. Under which of the following circumstances should the dosage of adenosine be reduced?
a.The patient is taking theophylline.
b.The patient is taking dipyridamole.
c.The patient has significant valvular regurgitation.
d.The patient has a significant left-to-right shunt.
4.Which of the following medications is contraindicated for use with dofetilide?
a.Digoxin
b.Diltiazem
c.Verapamil
d.Propranolol
5.Which of the following antiarrhythmic drugs may be more likely to have proarrhythmia at increased heart rates?
a.Sotalol
b.Flecainide
c.Quinidine
d.Dofetilide
6.Which of the following statements is true regarding antiarrhythmic drugs with reverse-use dependence?
a.Antiarrhythmic drugs with reverse-use dependence have greater efficacy for arrhythmia prevention than termination and have less risk for ventricular proarrhythmia at slower heart rates.
b.Antiarrhythmic drugs with reverse-use dependence have less efficacy for arrhythmia prevention than termination and have greater risk for ventricular proarrhythmia at slower heart rates.
c.Antiarrhythmic drugs with reverse-use dependence have greater efficacy for arrhythmia prevention than termination and have greater risk for ventricular proarrhythmia at slower heart rates.
d.Antiarrhythmic drugs with reverse-use dependence have less efficacy for arrhythmia prevention than termination and have less risk for ventricular proarrhythmia at slower heart rates.
7.Which of the following is true regarding the Cardiac Arrhythmia Suppression Trials (CAST I and II)?
a.The treatment drugs increased mortality for patients without heart disease.
b.All class IC antiarrhythmic drugs were found to decrease mortality.
c.The treatment drugs effectively suppressed premature ventricular complexes (PVCs).
d.The antiarrhythmic drugs studied were flecainide, propafenone, and moricizine.
8.Which of the following antiarrhythmic drugs is the most potent sodium channel blocker?
a.Flecainide
b.Lidocaine
c.Disopyramide
d.Procainamide
9.Which of the following effects is expected when administering adenosine to a patient with recent cardiac transplantation (denervated heart)?
a.No effect
b.Diminished effect
c.Enhanced effect
d.Delayed effect
10.A patient presents with regular narrow QRS tachycardia. A 12-lead electrocardiogram (ECG) demonstrates an r’ in lead V1 that was not seen on ECG when the patient was in sinus rhythm. An esophageal electrode shows a 1:1 atrial-to-ventricular relationship during tachycardia. The ventriculoatrial (VA) interval is measured as 55 milliseconds. Which of the following is the most likely diagnosis?
a.Orthodromic atrioventricular reentrant tachycardia (AVRT)
b.Atrial tachycardia
c.AV nodal reentrant tachycardia (AVNRT)
d.Permanent junctional reciprocating tachycardia (PJRT)
11.A 17-year-old patient who is known to have Wolff-Parkinson-White syndrome presents with a regular narrow complex tachycardia with a cycle length of 375 milliseconds (160 bpm) that occurred with a sudden onset. You note that there is a 1:1 atrial-to-ventricular relationship and that the RP interval is 100 milliseconds. The best initial treatment is
a.IV procainamide.
b.atropine.
c.vagal maneuvers.
d.catheter ablation.
12.A 25-year-old patient presents with the sudden onset of tachycardia and is found to have a regular narrow QRS tachycardia with a cycle length of 340 milliseconds (176 bpm). An ECG appears to show P waves visible just after each QRS complex. You place an esophageal electrode and confirm a 1:1 atrial-to-ventricular relationship with a VA interval of 110 milliseconds. During the tachycardia, there is spontaneous development of left bundle branch block (LBBB), and a slower tachycardia with a VA interval of 150 milliseconds is now seen. What is the most likely diagnosis for the second tachycardia?
a.AVNRT
b.Orthodromic AVRT using a right-sided accessory pathway
c.Orthodromic AVRT using a left-sided accessory pathway
d.Ventricular tachycardia (VT) with 1:1 VA conduction
13.A 65-year-old man presents after an arrest while eating at a local restaurant. On arrival, paramedics documented ventricular fibrillation (VF), and he was successfully resuscitated. He has a history of myocardial infarction (MI) and congestive heart failure (CHF). Serum electrolytes are remarkable only for mild hypokalemia. MI is ruled out by ECG and serial blood tests of myocardial enzymes. Subsequent evaluation includes cardiac catheterization, which shows severe three-vessel coronary artery disease (CAD) and severe left ventricular (LV) systolic dysfunction. A nuclear myocardial perfusion scan shows a large area of myocardial scar without significant viability in the territory of the left anterior descending coronary artery. The decision is made to treat the CAD medically. Which of the following is the best management strategy for his arrhythmia?
a.PO amiodarone
b.Implantable cardioverter defibrillator (ICD) implantation if an electrophysiologic (EP) study shows inducible VT or VF
c.ICD implantation
d.β-Blocker medication
14.A 55-year-old woman has CAD and moderately severe LV systolic dysfunction (LV ejection fraction, 34%). Routine ambulatory Holter monitoring shows asymptomatic frequent ventricular ectopy with PVCs and occasional runs of nonsustained VT. Which of the following statements about the management of this patient is true?
a.Implantation of an ICD is indicated.
b.Implantation of an ICD is indicated if an EP study shows inducible VT.
c.Treatment with amiodarone is indicated, and if the arrhythmia recurs, then an EP study is indicated.
d.No treatment is indicated unless the arrhythmia becomes symptomatic.
15.A patient arrives at the emergency department after experiencing multiple shocks from his ICD. The shocks were not preceded by any symptoms. He is noted to be in sinus rhythm on presentation, and, while on the monitor, he receives several more shocks from the ICD without any arrhythmias noted. Which of the following is the most appropriate initial step in the management of this patient?
a.Immediately arrange for a programmer for interrogation and reprogramming of the ICD.
b.Arrange for urgent surgery in the EP laboratory.
c.Initiate antiarrhythmic drug therapy.
d.Place a “donut” magnet over the ICD site.
16.Which of the following is most important for successful resuscitation of an adult patient with out-of-hospital cardiac arrest?
a.IV epinephrine
b.Early direct current (DC) shock defibrillation
c.IV antiarrhythmic drugs
d.Early intubation
17.Which of the following rhythms documented at the time of resuscitation from cardiac arrest carries the poorest prognosis for long-term survival?
a.Asystole
b.Electromechanical dissociation (EMD) or pulseless electrical activity (PEA)
c.VF
d.VT
18.Which of the following rhythm disturbances is most commonly documented for an adult with out-of-hospital sudden cardiac death resuscitated within the first 4 minutes after arrest?
a.Asystole
b.EMD or PEA
c.Monomorphic VT
d.VF
19.Which of the following treatment options has been most consistently shown to be effective for the primary prevention of sudden cardiac death in patients with CAD and recent MI?
a.D-Sotalol
b.β-Blocker medications
c.Amiodarone
d.Dofetilide
20.Which of the following is the most common condition associated with sudden cardiac death in the United States?
a.Hypertrophic cardiomyopathy
b.CAD
c.Valvular heart disease
d.Dilated cardiomyopathy
21.A 55-year-old man is referred for recurrent syncope. The episodes consist of a prodrome of weakness and nausea followed by loss of consciousness. Physical examination is unremarkable. ECG and exercise treadmill stress test were normal. Which of the following is the most appropriate next step?
a.EP study
b.Signal-averaged ECG
c.Head-upright tilt-table testing
d.Ambulatory Holter monitoring
22.A 40-year-old woman presents to the emergency department with tachycardia. An ECG shows regular narrow complex tachycardia at 160 bpm. Atrial activity is difficult to discern in the tracing, but during tachycardia, there appears to be an “r’” in lead V1 that is not present on an ECG during sinus rhythm recorded a few months earlier. Which of the following is the most likely diagnosis?
a.AVNRT
b.AVRT
c.Atrial tachycardia
d.Atrial flutter
23.An 80-year-old man with chronic AFib of 15 years’ duration is admitted with recurrent episodes of dizziness and a recent episode of syncope. He has normal LV function and no evidence of CAD. In-hospital telemetry confirms the presence of slow ventricular rate and frequent pauses (4 seconds) that correlate with his lightheadedness. His medications consist of warfarin sodium (Coumadin). The most appropriate course of action includes which of the following?
a.Reassuring the patient and instructing him to come back if he has recurrence of syncope
b.Prolonged monitoring with a loop recorder
c.EP testing to evaluate for ventricular arrhythmia
d.Permanent pacemaker implant
e.ICD implant
24.A decision was made in the previous case to proceed with a permanent pacemaker. Which would be the most suitable pacing modality?
a.Dual-chamber system programmed to DDDR
b.Dual-chamber system programmed to DDDR with mode switching
c.Dual-chamber system programmed to DDIR
d.Single-chamber system in the ventricle programmed to VVIR
e.Single-chamber system in the atrium programmed to AAIR
25.Which one of the following is true about “pacemaker syndrome”?
a.Symptoms usually include fatigue, dizziness, and hypotension.
b.It occurs equally in atrial-based and ventricular-based pacing systems.
c.It does not occur in patients who have 1:1 VA conduction.
d.It can be treated with fludrocortisone.
e.It is treated by increasing the VVI baseline pacing rate.
26.Of the following patients, who is the most likely to carry the diagnosis of sick sinus syndrome (SSS)?
a.A 65-year-old woman with a resting sinus arrhythmia varying from 70 to 85 bpm
b.A 30-year-old with sinus pauses 1.5 seconds in duration
c.A 20-year-old athletic man with sinus bradycardia at 25 bpm while sleeping
d.A 73-year-old man with persistent AFib and a ventricular rate of 40 bpm during peak treadmill test
e.A 70-year-old with sinus bradycardia and AV block secondary to a β-blocker overdose
27.A 76-year-old patient with dilated cardiomyopathy and LBBB on baseline ECG is undergoing evaluation for syncope. Placement of a catheter near his bundle during EP testing is most likely to
a.induce AFib.
b.induce VT.
c.perforate the atrium.
d.perforate the ventricle.
e.induce complete heart block (CHB).
28.A 25-year-old patient with a history of depression is brought to the emergency room after ingesting some of her mother’s prescription medications, including diltiazem and metoprolol. Her pulse rate is 25 bpm, and her BP is 90/50 mmHg. Her ECG shows sinus bradycardia and high-grade AV block. In preparation for temporary pacemaker placement, which of the following is most likely to be effective?
a.IV calcium gluconate
b.Isoproterenol infusion
c.IV atropine
d.IV magnesium sulfate
e.IV glucagon
29.A young patient is admitted to the intensive care unit with amitriptyline overdose. Three hours after gastric lavage, he develops hypotension and wide complex tachycardia that is recurrent despite cardioversion. Appropriate management includes which of the following?
a.IV bretylium
b.Temporary pacemaker with overdrive pacing
c.IV calcium gluconate
d.IV hypertonic sodium bicarbonate
e.IV magnesium sulfate
30.An 80-year-old undergoes dual-chamber pacemaker placement for CHB. Excellent ventricular and atrial capture thresholds were obtained at the time of the implant. The pacemaker programmed parameters are as follows: mode, DDD; lower rate, 70 bpm; upper rate, 130 bpm; atrial sensitivity, 0.25 mV (most sensitive setting); ventricular sensitivity, 1.00 mV; AV delay, 175 milliseconds; pace/sense configuration, bipolar. The next day, the following rhythm strip was recorded (Fig. 1.1): This rhythm strip shows
a.normal pacemaker function for the programmed parameters.
b.atrial noncapture.
c.ventricular noncapture.
d.atrial undersensing.
e.ventricular undersensing.
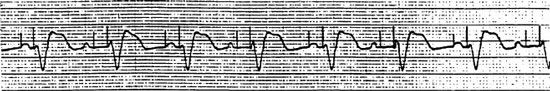
Figure 1.1
31.A 50-year-old man with chronic obstructive pulmonary disease related to chronic smoking presents to the emergency room with palpitations. ECG shows narrow QRS tachycardia at 165 bpm. His BP is 125/60 mmHg. Expiratory wheezes are heard on lung examination. His medications include albuterol inhaler and theophylline. The most appropriate initial treatment includes which of the following?
a.Adenosine IV bolus
b.Digoxin loading over 6 hours
c.Verapamil IV bolus
d.Propafenone IV bolus
e.Immediate cardioversion
32.A 55-year-old woman returns to the clinic after a recent dual-chamber pacemaker placement. She reports frequent palpitations and fatigue. These episodes last for several minutes before stopping. A Holter monitor recorded the following rhythm (Fig. 1.2): The pacemaker is programmed to mode DDD; lower rate, 80 bpm; upper rate, 150 bpm; AV delay, 200 milliseconds; postventricular atrial RP, 150 milliseconds. The latter part of this rhythm strip shows
a.VT induced by the pacemaker.
b.initiation of atrial tachycardia with atrial tracking.
c.pacemaker-mediated tachycardia.
d.pacemaker function failure with inappropriate rapid ventricular pacing.
e.artifact.
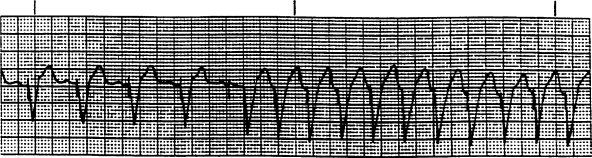
Figure 1.2
33.An 82-year-old man receives a dual-chamber pacemaker for SSS. Routine transtelephonic check (without and with magnet) shows the following strips (Fig. 1.3). Which of the following is true?
a.The pacing mode is VVI secondary to automatic mode switch.
b.There is consistent atrial capture on the magnet strip.
c.There is consistent ventricular capture.
d.Ventricular sensing cannot be determined by the available strips.
e.Atrial sensing cannot be determined by the available strips.
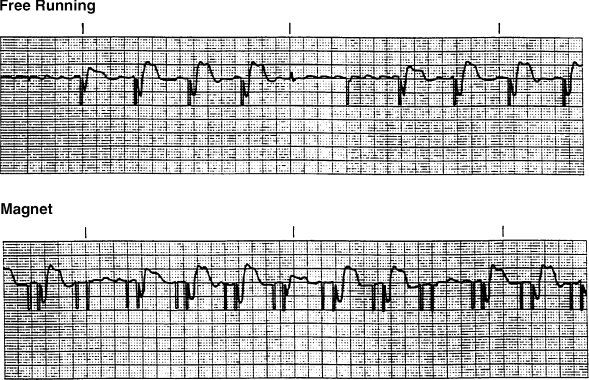
Figure 1.3
Questions 34–37
The following tracings (Figs. 1.4, 1.5, 1.6, and 1.7) are obtained during EP evaluation of AV conduction in different patients. HRA (high right atrium) and HBE (His bundle electrogram) are the intracardiac electrograms, recording from the high right atrium and the His bundle regions, respectively. Which of the following is true for these tracings?
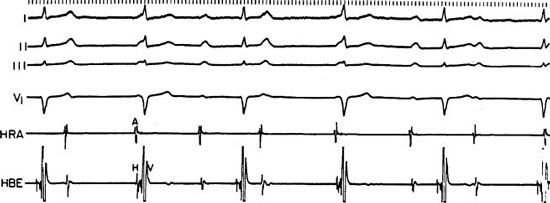
Figure 1.4
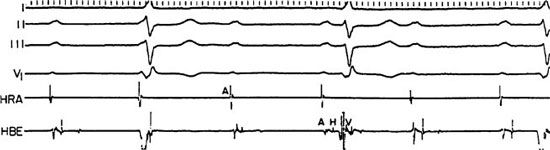
Figure 1.5
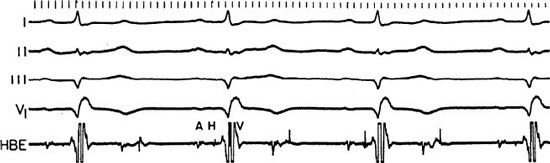
Figure 1.6

Figure 1.7
a.CHB at the level of the AV node
b.CHB at the infra-Hisian (below the His bundle) level
c.Second-degree AV block at the AV node level
d.Second-degree AV block at an infra-Hisian level
e.First-degree AV block
38.A 38-year-old woman with congenital CHB undergoes a dual-chamber permanent pacemaker. A 12-lead ECG obtained after the procedure shows normal sinus rhythm (NSR) with atrial tracking (a sense–V pace behavior). The ventricular-paced complex has a right bundle branch block (RBBB) morphology. Further evaluation should include
a.obtaining a portable anteroposterior chest X-ray (CXR) to evaluate lead position.
b.obtaining a two-view (anteroposterior and lateral) CXR to evaluate lead position.
c.repeating the 12-lead ECG.
d.requesting a pacemaker interrogation.
e.reassuring the patient without ordering further tests.
39.Which of the following is true regarding EP testing of the conduction system?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


