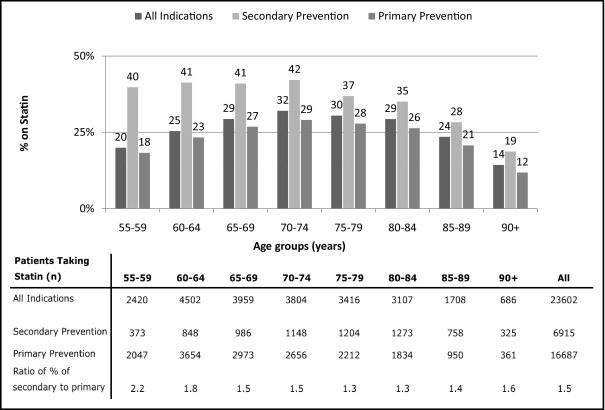
In patients aged ≥80 years without previous coronary artery disease, peripheral vascular disease, or cerebrovascular disease, no evidence has shown a benefit from statin therapy. We examined the prevalence of statin use in patients aged ≥80 years for the indication of primary prevention. We reviewed the comprehensive electronic health records at the Geisinger Health System in Pennsylvania for all patients aged >55 years with ≥1 primary care encounter from January 24, 2004 and December 31, 2009. The records were scrutinized for the use of a statin, active medical diagnoses, and laboratory values. Patients without a previous diagnosis of coronary artery disease, peripheral vascular disease, or cerebrovascular disease were considered to have a primary prevention indication for statin therapy. The prevalence of statin use was examined, and a multivariate analysis was conducted to determine the predictors of use. A total of 89,086 patients were included in the analysis, with 22,646 patients aged ≥80 years. Of all the patients, 26% were prescribed a statin, of whom, 71% (n = 16,687) received it for primary prevention. Of the 14,604 patients aged ≥80 years with a primary prevention indication, 3,145 (22%) received a statin. A plot of 5-year age cohorts from 55 to >90 years demonstrated an n -shaped relation between age and statin use for primary prevention (18%, 23%, 27%, 29%, 28%, 26%, 21%, and 12%, p <0.001). Compared to patients aged <65 years, the ratio of statin prescription for secondary to primary prevention was 31% lower in patients aged ≥80 years (1.3 vs 1.9). Those aged ≥80 years with a primary prevention indication had, with treatment, a mean low-density lipoprotein level of 84 ± 26 mg/dl. In conclusion, many patients aged ≥80 years receive statin therapy for primary prevention and are treated to aggressive low-density lipoprotein levels. Because the efficacy is uncertain and the potential adverse effects are many, we urgently need to define the cost, benefit, and risk of statin use in the very elderly.
By 2030, approximately 20 million people living in the United States will be ≥80 years old. In those aged 75 to 85 years, it is estimated that ≥33% of men and ≥20% of women will be taking a statin. Although there is good evidence for the benefits of secondary prevention in patients aged ≥80 years, limited data are available for statins as primary prevention therapy. The Third Report of the Expert Panel on the Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults has stated that for men aged >65 years and women aged >75 years, “clinical judgment assumes increased importance in [the] choice of LDL [low-density lipoprotein]-lowering therapies.” This statement simply reflects the paucity of evidence showing benefit in this age group. Given the lack of data, the first step is to establish the prevalence of statin therapy in the general population.
Methods
The present study was conducted at Geisinger Health System, an integrated delivery system that serves residents in 43 counties in central and northeastern Pennsylvania. All clinics have used the EpicCare electronic health record since 2001, and the electronic health record database contains information for >3 million patients.
The Geisinger Health System electronic health record was reviewed for eligible patients. All patients aged >55 years with ≥1 primary care encounter from January 24, 2004 to December 31, 2009 were included in the present study. Patients with a statin on their active medication list at their most recent clinical encounter were considered to be using a statin. The list of used statins included pravastatin, simvastatin, atorvastatin, lovastatin, rosuvastatin, and fluvastatin.
Patient problem lists, clinical encounter data, and medication-associated diagnoses were electronically reviewed to determine the prevalence of clinical diagnoses in this population. Specifically, patient encounters were reviewed for “International Classification of Diseases, 9th Revision, Clinical Modification” codes, including 410 to 414 (ischemic heart disease), 430 to 438 (cerebrovascular disease), 440 to 448 (diseases of the arteries, arterioles, or capillaries), 250.0 to 250.93 (diabetes mellitus), 401 to 405 (hypertension), and 272 (hyperlipidemia). The record was reviewed for previous or active smoking.
Patients with a diagnosis of coronary artery disease, peripheral vascular disease, or cerebrovascular disease were categorized as having a secondary prevention indication for statin use and those without were considered to have a nonsecondary or primary prevention indication.
From this database, information was also available to assess and calculate the Charlson co-morbidity index for all patients in the present study. The Charlson index predicts the 10-year mortality of a patient according to the diagnosis of a wide range of co-morbid conditions. Each condition is assigned a score of 1, 2, 3, or 6, depending on the risk of dying associated with that condition. The scores are then summed and given a total score that predicts mortality. A total of 17 co-morbidities were assessed in this index, including myocardial infarction, heart failure, peripheral vascular disease, cerebrovascular disease, dementia, chronic pulmonary disease, connective tissue disease, peptic ulcer disease, mild liver disease, diabetes without complications, diabetes with complications, paraplegia, renal disease, cancer, moderate or severe liver disease, metastatic cancer, and human immunodeficiency virus. These co-morbidities were used in a multivariate analysis to determine the predictors of statin use.
The lipid levels were reviewed when available (the data were available for >85% of the patients.) The patient demographics were also examined.
All analyses were performed using a standard statistical package (SPSS, version 16.0, SPSS, Chicago, Illinois). Continuous variables are expressed as the mean ± SD. Categorical variables are expressed as numbers and percentages. We performed univariate analyses of the continuous variables using a 2-tailed Student t test and chi-square test for categorical variables. One-way analysis of variance with a post hoc Bonferroni test was used to compare the mean values of the continuous variables among multiple groups. We calculated the predictors of statin use according to logistic regression analysis. Univariate and multivariate logistic regression models were developed to analyze the use of statins for primary and secondary prevention. Variables were inserted into the model as forward Wald conditional (i.e., only those variables that had clinical and statistical significance were included). P Values were considered significant at <0.05.
Results
A total of 89,086 patients were included in the analysis, with 22,646 patients aged ≥80 years. Of these, 23,602 (26%) were prescribed a statin, of whom, 16,687 (71%) received the statin for primary prevention and 6,915 (29%) for secondary prevention.
The prevalence of statin use in those aged ≥80 years relative to those aged 55 to 79 years was 24% versus 27% (5,501 of 22,646 vs 18,101 of 66,440 patients, p <0.001) with 22% versus 25% (3,145 of 14,604 vs 13,542 of 55,043 patients, p <0.001) taking a statin for primary prevention and 29% versus 40% (2,356 of 8,042 vs 4,559 of 11,387 patients, p <0.001) for secondary prevention. The prevalence of vascular disease and co-morbidities, as assessed by the Charlson index, was greater (1.7 vs 1.0, p <0.001) in the age ≥80-year cohort ( Table 1 ). Diabetes mellitus and hypertension were more prevalent in the older group, and hyperlipidemia and smoking history were less prevalent.
| Variable | All Patients (n = 89,086) | Age (years) | p Value | |
|---|---|---|---|---|
| 55–79 (n = 66,440) | ≥80 (n = 22,646) | |||
| Mean age (years) | 71 ± 10 | 67 ± 7 | 85 ± 4 | <0.001 |
| Women | 49,312 (55%) | 35,668 (54%) | 13,644 (60%) | <0.001 |
| Race | <0.001 | |||
| White | 87,485 (98%) | 65,016 (98%) | 22,469 (99%) | |
| Black | 633 (0.7%) | 574 (0.9%) | 59 (0.3%) | |
| Hispanic | 447 (0.5%) | 389 (0.6%) | 58 (0.3%) | |
| Asian American | 294 (0.3%) | 258 (0.4%) | 36 (0.2%) | |
| Coronary artery disease | 8,836 (10%) | 5,307 (8%) | 3,529 (16%) | <0.001 |
| Peripheral vascular disease | 6,373 (7%) | 3,717 (6%) | 2,656 (12%) | <0.001 |
| Cerebrovascular disease | 8,830 (10%) | 4,753 (7%) | 4,077 (18%) | <0.001 |
| Coronary artery disease, peripheral vascular disease, or cerebrovascular disease | 19,429 (22%) | 11,387 (17%) | 8,042 (36%) | <0.001 |
| Diabetes | 13,893 (16%) | 9,821 (15%) | 4,072 (18%) | <0.001 |
| Hypertension | 30,647 (34%) | 21,113 (32%) | 9,534 (42%) | <0.001 |
| Ever smoker | 44,146 (50%) | 34,608 (52%) | 9,538 (42%) | <0.001 |
| Hyperlipidemia | 25,058 (28%) | 19,007 (29%) | 6,051 (27%) | <0.001 |
| Mean Charlson index | 1.2 ± 1.4 | 1.0 ± 1.3 | 1.7 ± 1.5 | <0.001 |
| Prescribed statin | 23,602 (26%) | 18,101 (27%) | 5,501 (24%) | <0.001 |
| Primary prevention | 16,687 (24%) | 13,542 (25%) | 3,145 (22%) | <0.001 |
| Secondary prevention | 6,915 (36%) | 4,559 (40%) | 2,356 (29%) | <0.001 |
For primary prevention, a plot of the 5-year age cohorts ( Figure 1 ) from 55 to >90 years demonstrated an n -shaped relation between age and statin use (18%, 23%, 27%, 29%, 28%, 26%, 21%, 12%, p <0.001). Statin use for secondary prevention was significantly lower in patients aged ≥80 years, with a declining trend seen with increasing age. Compared to those aged <65 years, the ratio of statin prescription for secondary to primary prevention was 31% lower in the patients aged ≥80 years (1.3 vs 1.9).
Multivariate analysis showed patients with a greater Charlson co-morbidity index were less likely to be taking a statin for either primary prevention (relative risk [RR] 0.94, 95% confidence interval [CI] 0.91 to 0.97) or secondary prevention (RR 0.94, 95% CI 0.93 to 0.96). Specifically, those aged ≥80 years with a primary prevention indication were significantly less likely to be taking a statin if they had a diagnosis of dementia (RR 0.77, 95% CI 0.64 to 0.94), cancer (RR 0.83, 95% CI 0.74 to 0.92), chronic pulmonary disease (RR 0.57, 95% CI 0.50 to 0.66), mild liver disease (RR 0.13, 95% CI 0.04 to 0.47), connective tissue disease (RR 0.53, 95% CI 0.42 to 0.67) or heart failure (RR 0.63, 95% CI 0.54 to 0.73). All multivariate predictors of statin use in the primary prevention group are listed in Table 2 .
| Predictor | Univariate RR | 95% CI | p Value | Multivariate RR | 95% CI | p Value |
|---|---|---|---|---|---|---|
| Age (years) | 0.91 | 0.89–0.92 | <0.001 | 0.93 | 0.91–0.97 | <0.001 |
| Women | 1.23 | 1.13–1.34 | <0.001 | 1.64 | 1.48–1.81 | <0.001 |
| White | 1 | 1 | ||||
| Black | 1.63 | 0.84–3.14 | 0.143 | 2.59 | 1.18–5.65 | 0.02 |
| Hispanic | 0.52 | 0.20–1.33 | 0.172 | 0.55 | 0.21–1.48 | 0.28 |
| Asian American | 0.69 | 0.24–2.02 | 0.50 | 1.08 | 0.32–3.72 | 0.90 |
| Hypertension | 0.74 | 0.68–0.81 | <0.001 | 0.69 | 0.63–0.75 | <0.001 |
| Diabetes | 1.72 | 1.55–1.90 | <0.001 | 1.12 | 1.00–1.26 | 0.046 |
| Hyperlipidemia | 1.65 | 1.52–1.80 | <0.001 | 1.46 | 1.33–1.61 | <0.001 |
| Ever smoking | 1.01 | 0.93–1.10 | 0.84 | 1.05 | 0.95–1.16 | 0.31 |
| Low-density lipoprotein | 0.98 | 0.98–0.98 | <0.001 | 0.98 | 0.98–0.98 | <0.001 |
| Low-density lipoprotein group (mg/dl) | ||||||
| <70 | 1 | 1 | ||||
| 70–100 | 0.78 | 0.70–0.87 | <0.001 | 0.73 | 0.65–0.82 | <0.001 |
| 101–130 | 0.33 | 0.29–0.37 | <0.001 | 0.29 | 0.25–0.32 | <0.001 |
| 131–160 | 0.16 | 0.13–0.19 | <0.001 | 0.13 | 0.11–0.16 | <0.001 |
| 161–200 | 0.21 | 0.15–0.28 | <0.001 | 0.16 | 0.12–0.22 | <0.001 |
| >200 | 0.20 | 0.10–0.39 | <0.001 | 0.15 | 0.07–0.30 | <0.001 |
| Charlson index | 1.03 | 1.00–1.06 | 0.03 | 0.94 | 0.91–0.97 | <0.001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


