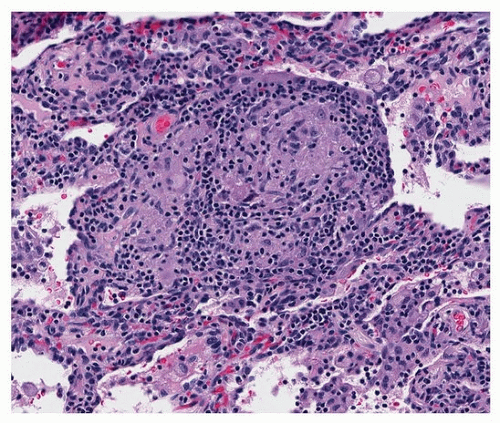
Well-formed granulomas are found in sarcoid or infections, usually fungal or mycobacterial. sarcoid and infections (
Table 9.1). There is a compact collection of epithelioid histiocytes with a discrete border (
Fig. 9.2) and a subpopulation of T lymphocytes. Sarcoid granulomas are found in a lymphatic distribution in the bronchovascular bundles, interlobular septa, and subpleural space. Fibrosis is a characteristic of sarcoid granulomas (
Fig. 9.3). Infectious granulomas are, in contrast, asymmetric and occur randomly in the parenchyma. Further, presence of significant lymphoplasmacytic inflammation favors an infectious etiology. Well-formed granulomas of any cause, but especially sarcoid, may contain mineral deposits (Schaumann bodies), which should not
be mistaken for pneumoconiosis (
Fig. 9.3). Asteroid bodies are also nonspecific features of well-formed granulomas (
Fig. 9.4).