Chapter 111
Aortoiliac
Extra-Anatomic Bypass
Joseph R. Schneider
The term extra-anatomic bypass refers to any bypass graft, autologous or otherwise that is placed in a site different from that of the arterial segment that is being bypassed. The term is imprecise at best since many common procedures, for example femorotibial bypass with in situ great saphenous vein or carotid artery to subclavian artery bypass might be considered “extra-anatomic.” However, the term extra-anatomic bypass is generally used to refer to procedures addressing disease of the aortoiliac and femoral arterial systems and include the basic procedures discussed in this chapter: femorofemoral bypass, axillofemoral bypass, obturator bypass, and thoracofemoral and supraceliac–to–iliofemoral bypass.
General Concepts
The basic situations for which extra-anatomic bypass procedures were developed include patients at unusually high risk for direct aortoiliac replacement (coronary artery atherosclerosis or other severe medical comorbidities), “hostile” abdomen (previous surgery or infection with adhesions, intestinal stomas, active intra-abdominal infection, or otherwise contaminated fields), infected prosthetic intra-abdominal vascular grafts, aortoenteric fistulae, and infected inguinal and infrainguinal arterial bypass grafts or other groin sepsis. These problems were apparent almost as soon as aortic and femoropopliteal vascular reconstructions were first performed in the 1950s and 1960s. Thus all of the basic procedures to be discussed were developed during that era. Although questions remain and data are contradictory regarding several aspects of outcomes with these extra-anatomic bypass procedures, the basic techniques are “mature.”
With respect to aortoiliac atherosclerotic occlusive disease, the rapid advances in endovascular therapy have included techniques that may be effective in patients who would previously have been treated with extra-anatomic bypass. However, younger patients with aortoiliac atherosclerosis, who would have been treated with direct aortofemoral bypass in the past, tend to have more discrete disease1–3 and patients with more discrete disease are precisely the group who tend to enjoy the best results with endovascular therapy. Older patients with more advanced comorbidities tend to have more diffuse atherosclerosis and for that reason tend to have less favorable results with endovascular therapy.4–9 Such older, higher-risk patients are more likely to require open surgical therapy, so extra-anatomic techniques would be expected to represent an increasing fraction of open surgical therapies for aortoiliac atherosclerosis. However, endovascular techniques continue to improve, to be applied to a rapidly increasing fraction of patients treated for iliac arterial occlusive disease including total occlusions,10 and may be applicable to a larger proportion of patients with diffuse aortoiliac disease in the future.11–13 Thus although the procedures themselves may be considered mature, their role and relative importance in the care of arterial problems is likely to continue to evolve.
History
Freeman and Leeds appear to have been the first to describe femorofemoral bypass,14 although a similar (ilioiliac) operation may have been performed earlier as part of a secondary procedure for iliac limb thrombosis after homograft repair for aortic bifurcation thrombosis and reported later by Oudot and Beaconsfield.15 However, Vetto’s 1962 report provided the first comprehensive description of a series of patients undergoing prosthetic femorofemoral bypass using techniques similar to those still in use today.16 Lewis17 described a truly remarkable subclavian artery to distal aortic homograft bypass as part of reconstruction for a patient with both a ruptured infrarenal aortic aneurysm and what seems likely to have been a type B aortic dissection,18 but the first uses of the axillary artery for inflow for axillofemoral extra-anatomic bypass appear to have been virtually simultaneous by Blaisdell and Hall19 and Louw.20 Blaisdell in particular continued to write about axillofemoral reconstruction and associated outcomes.21,22 Shaw and Baue included what are probably the first three cases of obturator bypass in an article describing suggested approaches to a number of infected arterial graft problems,23 although Courbier and Monties suggested the possibility of a transobturator graft route 3 years earlier.24 The first use of the thoracic aorta as the inflow for an extra-anatomic bypass was likely that described by Stevenson et al.25 Axillofemoral bypass and descending thoracic aorta–to–iliofemoral bypass (the latter, for simplicity, hereafter termed thoracofemoral bypass in this chapter) rapidly became important options for aortic prosthetic graft infection. For example, Fry and Lindenauer in 1967 reported the application of a number of these procedures, including at least one each axillofemoral, thoracofemoral, and supraceliac aorta–to–femoral bypass to cases of aortic graft infection.26 Each of these procedures has now been refined, and the experience with each is now sufficient to derive some general conclusions about their applicability and results.
Indications
The indications for extra-anatomic bypass are diverse and vary by the specific procedure contemplated. Femorofemoral and axillofemoral bypass are appropriate for patients with unilateral or bilateral chronic or acute arterial occlusive processes, most commonly atherosclerosis, with disease that is unfavorable for endovascular treatment and who are at high risk for aortofemoral bypass. Outcomes are particularly poor in patients with critical limb ischemia (CLI) who do not undergo arterial revascularization of some sort.27,28 Therefore, even high-risk patients with CLI due to aortoiliac occlusive disease will in most cases be suitable candidates for some sort of reconstruction, and femorofemoral and axillofemoral bypass are certainly among the interventions to be considered in such patients. These procedures may also be appropriate for revascularization in patients with active intra-abdominal infection (including “mycotic” aortic aneurysm or infected aortic prostheses), aortoenteric fistulae, or otherwise “hostile” abdomen that would be unusually difficult to treat with aortofemoral bypass. Obturator bypass is most commonly employed for femoral arterial reconstruction in patients with groin sepsis including primary vascular infection—for example, femoral mycotic aneurysm after puncture for a diagnostic or therapeutic endovascular procedure or recreational drug use, patients requiring removal of an infected arterial prosthesis in the groin, or patients with an otherwise “hostile” groin (e.g., after radiation therapy or previous surgery). Thoracofemoral and supraceliac aorta–to–iliofemoral bypass are most often employed to avoid reoperation in the infrarenal aorta after failure of standard aortofemoral bypass or after removal of infected prosthetic aortic grafts.
Contraindications
Femorofemoral and axillofemoral bypass are contraindicated in patients with extreme “medical” risk for surgery or with unusually short life expectancy. Obturator bypass with vein is a formidable procedure, and likely of greater magnitude than femorofemoral or axillofemoral bypass (or conventional femoropopliteal bypass), but the indications for obturator bypass are most often such that the only alternative may be to ligate the arteries in the groin and accept a substantial risk of major amputation. Consequently, the patient and surgeon may need to proceed with obturator bypass even if the patient is “high risk.” Thoracofemoral and supraceliac to iliofemoral bypass are both very formidable procedures, certainly equally or more “invasive” than conventional aortofemoral bypass, and they are inappropriate for patients at high risk for open abdominal or thoracic surgery. With respect to femorofemoral, axillofemoral, thoracofemoral, and supraceliac aorta–to–iliofemoral bypass, aortofemoral bypass remains the standard against which all other methods of reconstruction for iliac artery occlusive disease must be measured.29–34
Femorofemoral Crossover Bypass
Basic Concepts, Indications, and Patient Selection
Femorofemoral bypass depends on the capacity of one iliac arterial system to supply adequate blood flow to support both legs and is one possible reconstructive alternative for patients with symptoms related to unilateral stenosis or occlusion of a common or external iliac artery. Hemodynamic studies (see later) confirm that one iliac artery can support both legs, at least at rest, in the absence of flow limiting lesions in the planned “donor” iliac arterial system. Even a diseased donor iliac arterial system may be improved with endovascular techniques to allow a less invasive, yet effective femorofemoral bypass when a more invasive procedure would otherwise be required.
One attractive alternative to femorofemoral bypass is direct (ipsilateral) iliofemoral bypass. Kretschmer et al found no difference between femorofemoral bypass and unilateral iliofemoral bypass with respect to patency,35 but virtually all other published studies have found iliofemoral bypass to yield somewhat better patency than femorofemoral bypass, assuming an appropriate common iliac artery for inflow to the graft.36–45 Indeed, in a truly remarkable study, van der Vliet et al compared results of 184 unilateral iliac reconstructions (62% based on iliac artery inflow) and compared them with 350 contemporaneous patients undergoing aorta–to–bilateral iliac or femoral reconstruction over a 10-year time period and found no difference in patency between the groups, implying that iliofemoral bypass actually does yield results comparable to the “benchmark” aortofemoral bypass.46 However, even if the ipsilateral common iliac artery is relatively free of disease and would be an adequate inflow source for iliofemoral bypass, iliofemoral bypass is more invasive than femorofemoral bypass, and femorofemoral bypass may be preferred by some surgeons for that reason. Femorofemoral bypass may also be used as a component of endovascular repair of aortic aneurysm.47–57
Technique and Graft Configuration
Femorofemoral bypass is performed with the patient positioned supine. The operation can be performed with local infiltration anesthesia but is most often performed under spinal or general anesthesia. The abdomen is prepped along with the groin area and anterior thighs to allow access to the abdomen in case of unexpected findings during surgery. Longitudinal incisions are generally used to expose and control the femoral arteries on both sides. Although incisions parallel to the groin creases may be used, such oblique incisions are somewhat less versatile if exposure must be extended much more distal than the femoral artery bifurcation. General considerations described elsewhere in this text, as well as geometric considerations discussed in the following paragraphs, may affect the selection of the site of the arterial anastomoses.58
Femorofemoral bypass is certainly an operation of lesser magnitude than aortofemoral bypass, and the technique is regarded as simple by many surgeons. However, femorofemoral bypass, both as a stand-alone procedure and as part of an axillofemoral, thoracofemoral, or other bypass procedure, presents unique technical (geometric) challenges. The graft is tunneled from one groin incision to the other within the abdominal wall superior to the pubis (Fig. 111-1). The tunnel is created bluntly with fingers, a large clamp, or tubular tunneler. The prefascial subcutaneous plane will be the appropriate location for the graft tunnel in most patients, but a preperitoneal position59,60 may be elected or may be appropriate if unfavorable conditions exist in the abdominal wall such as prior surgery, radiation-damaged skin or other skin changes, an unusually thin subcutaneous fat layer, or even obesity predisposing to unfavorable graft geometry. The latter tunnel position may be associated with injury to bowel or urinary bladder61,62 and must be used with great caution, especially if there has been previous abdominal surgery. However, inflow for “crossover” bypasses may be provided in some cases by a contralateral iliac artery,36,63–68 and these iliac origin crossover grafts are usually most conveniently placed in the preperitoneal position. With the exception of Ng et al,69 most authors have found the patencies of these iliofemoral crossover bypasses to be comparable to or perhaps slightly better than femorofemoral bypasses. The outflow of such crossover grafts may be the popliteal or even tibial arteries70–72 or may be “sequential” grafts with an intermediate anastomosis to the femoral system in the groin, as well as a popliteal or other distal anastomosis to address both “inflow” (aortoiliac) and “outflow” (femoropopliteal) disease, especially in the setting of tissue loss due to multilevel disease.73,74 Even more unusual presentations may be addressed using a transperineal graft route.75–80 Readers are directed to the original publications for a more detailed description of these approaches.
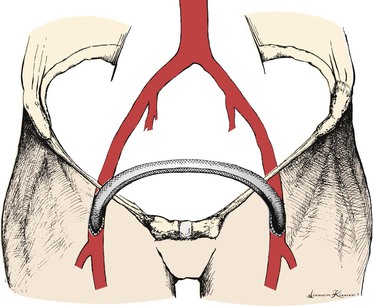
Figure 111-1 Standard “inverted C,” perhaps better termed “inverted U” configuration of femorofemoral bypass graft.
The graft is roughly confined to a plane tipped forward superiorly from the coronal plane to an extent that varies considerably with patient habitus. Anastomoses are made to some component of the femoral arterial system and are “end-to-side” in nearly all cases so that the graft is directed roughly longitudinally at the anastomoses. Whether the graft is configured as an “inverted C”81 (see Fig. 111-1; perhaps better termed “inverted U” and preferred by most surgeons) or a “lazy S,”82 the graft will make two abrupt changes in direction within the tipped-from-coronal plane just described. The likelihood of kinking can be reduced by using a slight excess of graft material, which reduces the tendency of the graft to kink at the “heel” of the anastomoses and by making the tunnel as a continuous curve between the groin incisions and several centimeters superior to the proposed anastomoses to try to increase the radii of the graft curves transitioning from a roughly longitudinal direction to a transverse direction coursing from one groin to the other.
The tendency of the graft to kink within the sagittal plane is a separate concern. The protuberant abdomen presents a problem not encountered in the aortofemoral graft that parallels the distal external iliac artery and emerges from beneath the inguinal ligament. The more obese or more protuberant the abdomen, the more the plane of the graft is tipped forward from coronal within the sagittal plane. This tends to cause the angle between the graft and the native artery to become less acute and, thereby, to cause a standard-length end-to-side anastomosis (roughly 3 times as long as the graft diameter) to kink in the sagittal plane. This can usually be prevented by making a shorter femoral arteriotomy (and anastomosis) or by making the anastomosis to a more distal part of the femoral arterial system, which has the effect of bringing the graft and the femoral artery into a more parallel (and desirable) relationship. Extending the anastomosis(es) at least partially onto the deep femoral artery may also be very helpful in reducing the tendency of the graft to kink in both the sagittal and coronal planes.
Systemic heparin is administered after completion of dissection and tunneling. Endarterectomized superficial femoral artery was used in Freeman and Leeds’ first femorofemoral bypass,14 and autologous vein grafts were common and even preferred conduits in some surgeons’ early experiences with femorofemoral bypass.83–85 A prosthetic graft is now used in nearly all cases, although almost every reported series of femorofemoral grafts has a few constructed of vein or other autologous vessel, generally placed in situations with high concern for infection.14,60,86–91 Another alternative, especially in the face of infection, is the use of femoral popliteal vein. D’Addio et al reported excellent results with femoral popliteal vein conduit in 54 patients, 16 of whom were undergoing femorofemoral bypass as the sole procedure.92 Either anastomosis may be performed first when using prosthetic conduits, but we would perform the donor anastomosis first when using venous conduits so that the presence of one or more competent valves in the conduit would not interfere with flushing just before completion of the second (recipient) anastomosis. Great care must be taken to allow some redundancy in the graft as noted earlier. It is very important to confirm enhancement of flow in the recipient vessels and continued flow in the outflow vessels beyond the donor side anastomosis using a continuous wave Doppler or other suitable test after anastomoses are completed and all clamps are removed.
Results
The perioperative mortality associated with femorofemoral bypass is highly dependent on patient selection but should be well under 5% in elective operations. Patients undergoing femorofemoral bypass are likely to have somewhat less advanced comorbidities and are consequently likely to enjoy longer survival than patients undergoing axillofemoral bypass. For example, we estimated patient survival of 71% for femorofemoral versus 35% for axillofemoral bypass at 3 years in our previous reports.93,94 Furthermore, far more patients appear to undergo femorofemoral than axillofemoral bypass procedures (for example, more than 4 times as many femorofemoral bypasses compared with axillofemoral bypasses were performed in Johnson and Lee’s prospective study95). Consequently, reports including 5-year results are much more common for femorofemoral bypass, allowing more confident assessment of long-term performance. We suggested in the sixth edition of this textbook that primary and secondary patency for femorofemoral bypass at 3 to 5 years should be expected to be about 60% and 70%, respectively,93,96–98 but results appear to have improved somewhat since that time. Ricco and Probst reported the results of a multicenter comparison of femorofemoral–to–inline (aortofemoral or iliofemoral) bypass and have also tabulated results of previously published studies of femorofemoral bypass including at least 40 patients, follow-up of at least 5 years, and with life-table estimates of graft patency at 5 years.45 Table 111-1 is modified from those tabulations to include only reports that also provide the number of grafts at risk at 5 years and with the addition of some previous and subsequent articles that also qualify.* This table demonstrates some variability in the patency estimates among these studies, likely due to diversity with respect to risk factors such as the fraction of patients with critical limb ischemia and failed previous aortofemoral bypass, which as noted elsewhere, can significantly affect femorofemoral graft patency. This variation is much less than is seen with axillofemoral bypass (see later). These tabulated data allow calculation of a weighted-average estimate of 5-year primary patency of 66%; however, a similar calculation confined to reports after the year 2000 yields a weighted-average estimate of 72%.
Table 111-1
Femorofemoral Bypass Patency
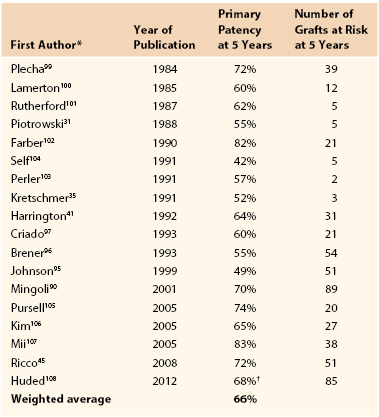
* Previously reported studies of femorofemoral bypass including at least 40 patients, follow-up of at least 5 years, and with life-table estimates of 5 year primary patency that appear to be compliant with current reporting standards.261,262
† Composite of femorofemoral bypass subjects with no adjunctive inflow (n = 74 at 5 years) and those with endovascular adjunctive inflow (n = 11 at 5 years) procedure.
Modified from Ricco J-B, et al: Long-term results of a multicenter randomized study on direct versus crossover bypass for unilateral iliac artery occlusive disease. J Vasc Surg 47:45-54, 2008.
Causes of Failure
The causes of extra-anatomic bypass graft failure are elusive, but are likely to include progression of disease in both inflow and outflow arteries. Although some early authors may have viewed femorofemoral bypass as a durable procedure not vulnerable to progression of disease109,110 and da Gama actually suggested that the donor artery enlarges over time after placement of an extra-anatomic bypass,111 other early adopters viewed femorofemoral bypass to be at risk from progression of disease in the donor iliac system.112,113
Surveillance
The role of noninvasive surveillance of femorofemoral and other extra-anatomic bypass grafts remains unclear, but Stone et al presented a unique exploration of the possible predictive value of duplex scan surveillance and concluded that a duplex scan estimated peak systolic velocity of greater than 300 cm/sec in the inflow artery or a midgraft peak systolic velocity less than 60 cm/sec were predictive of impending graft thrombosis.114 Early experience since adopting this approach in our practice seems to confirm the findings of Stone et al, although it should be noted that these findings have not been confirmed by others.
Effect of Surgical Indications and Patient Characteristics
Pursell et al noted a trend toward better patency in claudicants, consistent with the observation in virtually every other lower extremity arterial intervention.105 In contrast, Criado et al and, in what is among the largest, longest, and most completely followed series on femorofemoral bypasses, Brener et al noted no apparent difference in femorofemoral bypass patency comparing claudicants to patients with CLI.96,97 Our previous investigation actually suggested a trend toward reduced patency in patients with claudication compared with those with CLI, although the trend was not significant and would be difficult to explain except as a result of random error,93 and Huded et al’s recent report including data from our original publication found no difference between patency in claudicants versus subjects with CLI.108 On balance, it appears likely that results in claudicants are as good or better than those in subjects with critical limb ischemia, but not comparable to those after aortofemoral bypass.
Femorofemoral bypass is one of many methods of treating patients with symptomatic occlusion of one limb of a previously placed aortobifemoral graft.65,115,116 Although most authors have reported results in these patients to be inferior to those in patients undergoing primary femorofemoral bypass,87,93,96,101,117–119 others have described more favorable results.120–124 Most patients who suffer thrombosis of an aortobifemoral graft limb will be quite symptomatic and require urgent intervention.115,125–128 Femorofemoral bypass is one option, and the surgeon and patient may need to accept the prospect of a greater risk of subsequent failure in exchange for more expedient reperfusion of the leg. We have also noted a trend toward an inverse relationship between age and patency for femorofemoral bypass.93 However, we observed a similar trend after aortobifemoral bypass and this may represent the effect of more aggressive biology of atherosclerosis in patients who require intervention at a younger age.
Femorofemoral bypass has also been used as part of endovascular aneurysm repair using aortouniiliac systems.47–57 Local femoral wound complications have been a concern in several of these publications. However, patency of the femorofemoral graft in such patients has been excellent and clearly better than in those patients treated for occlusive disease. These results will be described in more detail in chapters dedicated to endovascular aneurysm repair.
Femorofemoral bypass was first used in patients considered unfit for aortofemoral bypass.129 However, the relative ease of the procedure and the substantially lower level of physiologic insult to the patient prompted many to extend the procedure to better risk patients who would be candidates for aortofemoral bypass.96,101,119,130–134 Femorofemoral bypass may also be preferred by some patients and surgeons because the risk of erectile dysfunction in men is likely lower than after aortofemoral bypass.67,87,93,135–137 We are aware of no randomized prospective comparisons of femorofemoral versus aortofemoral bypass, and even contemporaneous case control studies are unusual. We previously examined the results of patients who would have been candidates for aortofemoral bypass, but who instead underwent femorofemoral bypass, and we compared these results with patients undergoing aortofemoral bypass during the same time period in the same institution. The results of femorofemoral bypass, even in these good-risk patients, were clearly inferior to the results in patients undergoing aortofemoral bypass.93 Mingoli et al retrospectively reviewed and compared the performance of femorofemoral and aortofemoral bypass in two institutions between 1973 and 1993 and found no differences.138 However, this latter study must be considered unique since other studies of femorofemoral bypass consistently report inferior patency when compared with contemporaneous studies of aortofemoral bypass. Furthermore, many of the patients undergoing aortofemoral bypass in the past would be more appropriately treated with transluminal balloon angioplasty or iliofemoral bypass today, and it is unlikely that such a study could be repeated in a single institution today. In practice, it is rare that patient characteristics and arterial anatomy leave only two alternatives, femorofemoral or aortofemoral bypass, but when this is the case we continue to recommend the former for poor-risk patients and the latter for good-risk patients.
Effect of Graft Material and External Support
Most femorofemoral grafts have been constructed of prosthetic material. Dacron (polyester) was used almost exclusively until expanded polytetrafluoroethylene (ePTFE) became available. It is difficult to determine whether either of these classes of materials dominate femorofemoral bypass today. We could find no convincing evidence that either ePTFE or externally supported polytetrafluoroethylene (xPTFE) is superior to polyester grafts as measured by patency and hemodynamic performance. We are aware of no published data regarding the PTFE grafts with support within the wall (Gore Intering, W.L. Gore, Flagstaff, Ariz) in this application. At least one study found a trend toward inferior patency for ePTFE femorofemoral grafts.97 However, the remainder of published articles have reported comparable patency results using PTFE and polyester grafts in this application.45,90,95,139,140 Thus it currently appears that surgeons may choose either polyester or PTFE grafts and expect similar outcomes.
External or internal support is certainly a plausible contributor to improving the performance of femorofemoral and other subcutaneous bypass grafts. However, with the exception of Mingoli et al, who found an advantage of external support in a retrospective study including both polyester and PTFE grafts,90 we are aware of no clear evidence that external support provides superior outcomes in this application. Indeed, Kim et al106 reported results with mostly unsupported ePTFE grafts (Y.W. Kim, personal communication) that are indistinguishable from those with xPTFE in a report by Mingoli et al. Pursell et al also reported excellent results using unsupported polyester grafts (R.B. Galland, personal communication).105 Finally, we examined a series of 6-, 7-, 8-, and 10-mm diameter ePTFE grafts and could detect no relationship between diameter and hemodynamic performance or patency,93 findings confirmed by Ricco and Probst.45 Consequently, I have chosen to use 6-mm diameter xPTFE or Intering PTFE grafts for convenience and the possibility of decreased infection risk when performing femorofemoral bypass, but the hemodynamic performance and patency profiles of the available prosthetic grafts are probably indistinguishable in this application.
Hemodynamic Considerations
Many surgeons have been concerned that one iliac artery could not adequately supply blood flow to both legs or that the femorofemoral graft could “steal” from the donor limb and produce new or worsened symptoms of ischemia in the donor limb.85,86,113,141 Ehrenfeld et al showed that the capacity of a healthy iliac artery in an animal model far exceeds the resting flow requirements of both legs.141 Several authors have investigated the hemodynamic performance of the femorofemoral graft in patients and have concluded that there is rarely, if ever any significant deleterious effect on the donor limb and that the recipient limb remains well reperfused as long as there is no hemodynamically significant lesion in the donor iliac arterial system.60,130,142–144 The conclusions of these authors have dominated thought about femorofemoral graft hemodynamics to the present day. However, others have detected a slight fall in the mean resting ankle pressure on the donor side, a finding subsequently duplicated by several authors.60,93,143,145,146 Investigators for Veterans Affairs Cooperative Study 141 noted that the combination of hemodynamic deterioration and clinical symptoms of steal was present in only 3% of patients, although a much higher fraction of patients developed hemodynamic evidence of donor limb steal at rest, and angiographic findings did not predict the occurrence of donor limb steal.147 Harris et al made the remarkable observation that 45% of patients suffered deterioration in donor limb hemodynamics under exercise conditions despite normal resting donor limb hemodynamics after femorofemoral bypass.148 However, on balance, the evidence supports the contention that although some fall in donor limb pressure may occur after femorofemoral bypass, the donor limb is not functionally adversely affected by placement of a femorofemoral bypass as long there is no hemodynamically significant lesion in the donor iliac arterial system.
Significance of Iliac Artery “Inflow” Lesions.
Assessment of the hemodynamic significance of angiographically detected stenoses in the prospective donor iliac arteries has also been a topic of great interest in patients considered for femorofemoral bypass. Angiography alone is unreliable with respect to detection and assessment of hemodynamic significance of aortoiliac arterial disease.82,143,149–155 The increased flow in a donor arterial system after a bypass may unmask previously hemodynamically occult lesions.149,154,156 Sako was probably the first author to report the use of directly measured femoral artery pressures at rest and after injection of papaverine, a potent arterial vasodilator, to assess the capacity of the iliac arterial inflow to support a significant increase in flow.157 The test was subsequently further evaluated by Flanigan et al.158 The test as described by Flanigan is performed by directly measuring both systemic pressure and the arterial pressure in the proposed “donor” femoral artery before and after injection of 30 mg of papaverine into the femoral artery and has been used to predict whether an angiographically detected iliac lesion is of clinical importance when selecting “inflow” versus “outflow” reconstructive procedures or to determine whether an iliac artery will support a femorofemoral bypass. Flanigan et al found that femoral pressures more than 15% less than radial or brachial pressures were associated with an unsatisfactory outcome.
The concept of a physiologic test to predict how a potential donor iliac arterial system would behave under the stress of supporting two legs instead of just one is quite appealing. However, Archie has pointed out that only one study158 has examined the predictive value of the papaverine test.82 Furthermore, the technique has not been standardized. “Papaverine tests” are often performed with vasodilators other than papaverine, typically nitroglycerin or tolazoline. I have not been able to find literature to confirm that tests performed with other vasodilators are valid. I have also observed the test being performed without a separate radial artery or other catheter to measure systemic pressure during the test. This may cause a false positive result since systemic pressure often falls briefly but significantly during the 1 or 2 minutes immediately after injection of papaverine into the femoral artery. Finally, Flanigan stressed the importance of Doppler confirmation of increased flow in the proposed donor femoral arteries after papaverine injection, an often neglected portion of the test.158 Absence of such an increase in flow implies a technical problem with the test or significant occlusive disease limiting femoral outflow on the donor side and is likely to lead to a false negative test.
Archie has reported the largest and most detailed study of papaverine testing and its value in femorofemoral bypass.82 He found the test’s sensitivity and specificity inadequate to be reliable. However, despite the concerns expressed so eloquently by Archie, his work focused on the value of papaverine test data to predict patency and hemodynamic results as assessed in the noninvasive vascular laboratory. The value of papaverine testing as a predictor of relief of symptoms after femorofemoral bypass has not been so carefully examined. Thus we have continued to employ papaverine testing as one decision-making factor in femorofemoral bypass, particularly when balloon angioplasty of the donor iliac system is used, although we have devalued the test’s importance in view of Archie’s work.
Hemodynamic Results.
The ability of femorofemoral bypass to normalize perfusion of the recipient limb is more in question. Recipient limb perfusion is predictably improved by technically successful femorofemoral bypasses with appropriate anatomy.146 However, many surgeons have noted a significant number of clinical failures of femorofemoral bypass as measured by persistent claudication, rest pain, or failure to heal gangrenous lesions.145,159 The Veterans Affairs Cooperative Study 141 study cited earlier included more than 300 patients, clearly the largest study of femorofemoral hemodynamics to date, but these researchers presented no information about exercise testing of these patients.147 We previously examined the postoperative resting hemodynamics of femorofemoral bypass in 91 patients and concluded that recipient limb pressures would not be normal even at rest with completely normal femoral and other infrainguinal outflow vessels and as noted earlier; this finding was independent of the diameter of the graft used.93 Despite less than complete normalization of hemodynamics, femorofemoral bypass will in most cases provide adequate improvement in perfusion to maintain the limb in patients with critical limb ischemia.136,160 Although many surgeons view femorofemoral bypass as a satisfactory treatment for claudication,96,135,161–163 the persistent resting hemodynamic abnormalities in the recipient limb after femorofemoral bypass raise concern that it will perform poorly under exercise conditions.93,119,148 For this reason, we recommend inline revascularization for claudicants, which is usually possible with current interventional techniques.
Angioplasty of “Donor” Iliac Artery Before Femorofemoral Bypass
Successful femorofemoral bypass is highly dependent on a hemodynamically satisfactory donor iliac arterial system. Endovascular intervention for selected iliac artery lesions provides excellent short- and long-term results in terms of hemodynamic improvement and patency, as discussed in Chapter 112. It is not surprising that endovascular procedures to improve suboptimal donor iliac arteries might be considered before or concomitant with femorofemoral bypass. Porter et al164 described two patients who underwent graduated dilation (as previously described by Porter’s coauthor Dotter et al165) of the donor iliac artery before femorofemoral bypass with satisfactory early results in both. This procedure was performed before the development of balloon angioplasty by Grüntzig166,167 and others. Several authors have reported experience with transluminal balloon angioplasty before or concomitant with femorofemoral bypass.93,96,97,108,168–176 With rare exceptions,39,96,108 results of these studies have generally supported the view that donor iliac artery balloon angioplasty with stenting in selected cases is associated with a satisfactory hemodynamic outcome and patency rate. Furthermore, the results of balloon angioplasty have probably improved since the initial studies were published.175 On balance, it appears that as long as the donor iliac lesion would be considered favorable for angioplasty apart from the proposed femorofemoral bypass (ideally a short, minimally calcified lesion of the common iliac artery), then it is reasonable to proceed with angioplasty of the donor iliac artery and femorofemoral bypass.
Effect of Outflow Disease
Vascular surgeons recognized the critical importance of outflow and particularly the deep femoral artery very early in the experience with aortofemoral reconstruction.177–180 This principle is almost certainly applicable to extra-anatomic bypass as well. As with other operations for iliac arterial occlusive disease, many surgeons have suspected that disease of the femoral outflow arteries has a major impact on long-term femorofemoral bypass patency.* However, the patency of the superficial femoral artery has been found by many other authors to have no detectable impact on long-term patency.87,93,96,97,182 Ensuring outflow to at least one healthy artery, either the superficial femoral or more often the deep femoral artery, appears to provide adequate outflow to support patency, just as seems the case with direct aortofemoral bypass.93,183,184 Some have argued that routine “profundaplasty” is indicated in “inflow” operations including femorofemoral, axillofemoral, and aortofemoral bypass,185 but this probably has no impact on hemodynamic performance or patency in the absence of significant deep femoral origin stenosis.34 The ability to pass a 3.5-mm diameter probe into the outflow artery after completing the “toe” portion but before completion of the anastomosis is reassuring with respect to the adequacy of outflow, and we have always confirmed that this maneuver could be accomplished before completing any “inflow” operation. On balance, despite our own previous observations, I believe that the quality of outflow may affect patency, but I also believe that maneuvers to ensure the best possible outflow are likely to minimize this effect.
Complications
Complications of femorofemoral bypass are those common to nearly all arterial operations including those discussed in Section 8 (Complications) of this text. Complications relatively unique to femorofemoral bypass include possible perforation of the bladder or intraperitoneal viscera during creation of the graft tunnel, particularly when a preperitoneal tunnel is used,61,62 although transvesical and transbowel passage of conventional aortofemoral grafts have also been reported.186
Axillofemoral Bypass
Basic Concepts, Indications, and Patient Selection
Axillofemoral bypass depends on the ability of a healthy axillary artery to supply adequate blood to the ipsilateral arm and one or both legs, at least at rest. With the exception of occasional use as treatment of patients with aortic coarctation,187–189 axillofemoral bypass is used almost exclusively as treatment for patients with primary or secondary disease of the infrarenal aorta or iliac arteries. Axillofemoral bypass, just as any other method of intervention for primary or secondary infrarenal aortoiliac disease, must be judged against aortofemoral bypass.30,32–34 Axillofemoral bypass is an essential tool for treatment of many patients with infected aorta or prosthetic arterial grafts or aortoenteric fistulae,190–199 although in situ alternatives, discussed in Section 8 (Complications) and elsewhere in this text, have been proposed even for these patients.199–207 Early experience demonstrated axillofemoral bypass to be an excellent alternative for frail, older adult patients with bilateral iliac artery disease and those with other comorbidities such as multiple prior abdominal operations, abdominal stomas, or prior radiation therapy.86,132,146,208–221 However, the choice between aortofemoral and axillofemoral bypass is often less than clear. The definition of “high risk” is quite subjective, and the threshold for choosing axillofemoral over aortofemoral bypass is likely to vary significantly among surgeons. For example, approximately 25% of our open reconstructions for bilateral iliac artery occlusive disease were axillofemoral bypasses (and we were criticized for this “high ratio” when we presented our work in 1991),94,222 whereas Hepp et al performed axillofemoral bypass about 10 times as often as aortofemoral bypass.223 This has led to markedly different profiles of patient samples in published series of axillofemoral bypass, a topic that will be further in the following section.
Technique and Graft Configuration
Axillofemoral bypass is nearly always performed under general anesthesia.224 We have on rare occasions performed the entire operation with local anesthesia and sedation, but the exploration of the axillary artery and tunneling of the axillofemoral graft segment are difficult to perform under such circumstances. The operation may be expedited by the use of two operating teams, especially for axillobifemoral bypass. Either axillary artery may be an appropriate donor unless there is disease in the subclavian or axillary artery, although the right side is preferred in cases of aortic infection since subsequent remedial operations may involve left flank or thoracic exposures. We have approached this question by measuring blood pressures in both arms and recording continuous-wave Doppler waveforms in the brachial arteries. If a systolic pressure discrepancy of 10 mm Hg or greater exists between the arms, the axillary artery on the side with the higher blood pressure is chosen.
We insist on a triphasic Doppler waveform in the brachial artery in the proposed donor limb. Some authors have recommended routine preoperative arch and subclavian arteriography, citing a substantial frequency of occult disease in the axillosubclavian arterial system of patients considered for axillofemoral bypass.225 If both axillary arteries appear hemodynamically adequate to support axillofemoral bypass, we generally choose the arm ipsilateral to the patient’s more ischemic lower extremity, even when performing axillobifemoral bypass. However, the contralateral axillary artery may be used as the inflow even for axillounifemoral bypass if required by the circumstances. In the case of infection, it may occasionally be necessary to place bilateral axillounifemoral or axillodistal grafts,226 for instance, to avoid infected groin wounds. These choices are often made on the basis of other practical issues—for example, to avoid stomas or other pathology or to avoid placing the graft on the side preferred by the patient for sleeping. We would discourage placement of an axillofemoral graft on the side of a patent arteriovenous hemodialysis fistula, although we are unaware of any objective examination of the results of such procedures. Intraoperative arterial pressure-monitoring catheters should generally be placed in the nondonor arm.
Some surgeons perform the operation with the donor side arm at the patient’s side, but we prefer a supine position with the arm abducted to 90 degrees on the donor side. We also place a rolled towel under the patient on that same side to lift the torso several centimeters from the operating table deck. We believe these maneuvers improve exposure of the most medial portion of the axillary artery and allow visualization of the flank and lateral chest wall while passing the graft tunneler. We have used the 65-cm Gore tubular tunneler (W.L. Gore, Flagstaff, Ariz) and found that it allows easy passage of the axillofemoral graft limb without an intermediate incision in the flank. Femorofemoral limbs are positioned using the same approach described previously for isolated femorofemoral bypass. We have always draped widely to allow thoracotomy, sternotomy, or celiotomy, if necessary, to manage intraoperative bleeding or other complications that would dictate these approaches (Fig. 111-2), although we have never found it necessary to perform any of these maneuvers.
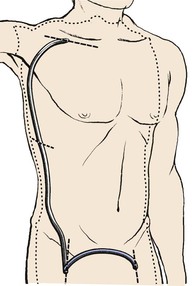
Figure 111-2 Typical area of exposure for an axillobifemoral bypass graft. The right axillary artery is the donor artery in this case. The intermediate incision in the right lower chest or upper flank is generally unnecessary if an appropriate tunneler is used.
Axillary Anastomosis
A transverse infraclavicular incision is carried through the clavipectoral fascia, exposing the pectoralis major muscle. The pectoralis major muscle fibers are pushed superiorly and inferiorly exposing the deep fascia and beneath that, the fat containing the axillary vein, artery, and brachial plexus elements. The axillary artery is exposed from the clavicle medially to the pectoralis minor muscle laterally, often requiring ligation of crossing veins or small arterial branches. The axillosubclavian arteries are considerably more fragile than the femoral arteries and care must be taken not to injure them or the adjacent veins and brachial plexus elements during dissection or during placement of retractors or vascular clamps. Similarly, care must be taken when performing anastomoses to the axillary arteries since sutures are much more likely to pull through these more fragile vessels. Conventional longitudinal or oblique groin incisions are used for femoral artery exposure.
Some early adopters of axillofemoral bypass recommended proximal anastomosis to the third portion of the axillary artery (lateral to the pectoralis minor muscle) since that portion of the artery is so accessible.208,214,218,227 However, Blaisdell21,228 from the beginning of his experience, and others since that time, have stressed medial placement of the axillary anastomosis on the first portion of the axillary artery (medial to the pectoralis minor muscle) to avoid tension (see next section). We have generally placed the graft posterior to the pectoralis minor muscle unless the patient has had prior axillary surgery, but placement of the axillary end of the graft anterior or posterior to the pectoralis minor muscle is probably unimportant with respect to results. It is far more important to place the axillary-graft anastomosis as medially as possible to avoid tension on the axillary anastomosis when the arm is abducted.229 Furthermore, medial placement of the axillary anastomosis eliminates the need to divide the pectoralis minor muscle in most cases. Leaving a slight excess length of graft in the axilla has also been advocated to reduce the likelihood of tension on the anastomosis.230,231 The axillofemoral graft must be tunneled subcutaneously in the midaxillary line to prevent kinking of the graft with torso flexion or kinking over the costal margin, which tends to be more prominent anteriorly than in the midaxillary line. Care must also be taken to avoid injury to the neurovascular structures of the axilla during tunneling.
Femoral Anastomoses
Systemic heparin is given after graft tunneling. The proximal-end-graft to side-axillary artery anastomosis is generally performed first. The order of distal anastomoses for axillobifemoral grafts may vary depending on whether there are one or two surgeons. The distal anastomosis is conventionally performed end-to-side to an appropriate artery in the groin. It is important to ensure adequate outflow. In the case of axillobifemoral configuration, the femorofemoral component may be placed by “piggy-backing” the femorofemoral graft onto the distal anastomotic hood of the axillofemoral graft (Fig. 111-3A). Alternatively, the femorofemoral graft may be placed first as described earlier and the distal anastomosis of the axillofemoral component may be piggy-backed onto the ipsilateral femorofemoral graft anastomotic hood. Either of these two variations would qualify as an inverted U femorofemoral component and would maintain maximum flow throughout the axillofemoral component, a characteristic thought to be desirable with respect to graft patency. Femorofemoral graft components should be placed using the principles described earlier. Blaisdell22,232 and Rutherford et al233 have described alternative configurations that theoretically prevent competitive inflow from the native iliac arterial system on the side of the distal axillofemoral anastomosis and which may thereby decrease the risk of graft thrombosis due to stasis (Fig. 111-3B and 111-3C). In Figure 111-3B, the common femoral artery is divided superior to the distal axillofemoral anastomosis and the femorofemoral graft component is anastomosed end-to-end to the distal common femoral artery. In Figure 111-3C, the common femoral artery is divided as in Figure 111-3B, but the common femoral artery is anastomosed to the side of the axillofemoral graft, which is then continued from the right groin to the left groin for the left femoral anastomosis. This latter configuration has the potential advantage of reducing the total number of anastomoses from four to three. Another alternative approach has been advocated by Wittens et al.234 These authors have examined a variety of grafts with manufactured bifurcations for axillobifemoral reconstructions. They found that a graft with a flow divider similar to that in bifurcated aortobifemoral grafts provided both superior hemodynamic performance and patency, although I could not identify any published confirmatory data since the original publication in 1992 except Dr. Wittens’ later doctoral thesis.234,235 Thus I would consider this approach as potentially useful but unconfirmed at this time. Indeed, this configuration appears similar to that first used by Sauvage and Wood210 but later described as “incorrect” by the same group.81 These grafts would appear to have long ipsilateral and contralateral distal graft limbs beyond the graft bifurcation, contrary to the most typical strategy as mentioned earlier. Furthermore, such a configuration would seem to require either a much longer ipsilateral groin incision or a counter-incision on the ipsilateral flank to avoid kinking of the contralateral distal graft limb. It is very important to confirm enhancement of flow in the recipient vessels using a continuous wave Doppler or other suitable test after anastomoses are completed and all clamps are removed. It is also essential to confirm adequate blood flow in the donor arm beyond the axillary anastomosis by confirming a good radial pulse or satisfactory oxygen saturation as indicated by pulse oximetry in the hand with both the axillofemoral graft and axillary outflow vessels unclamped.
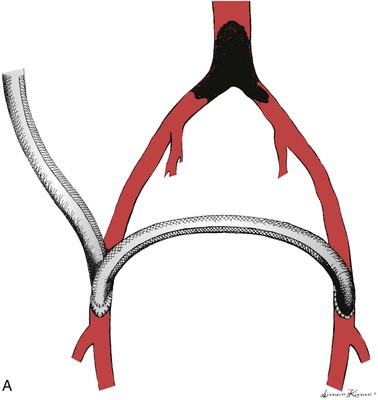
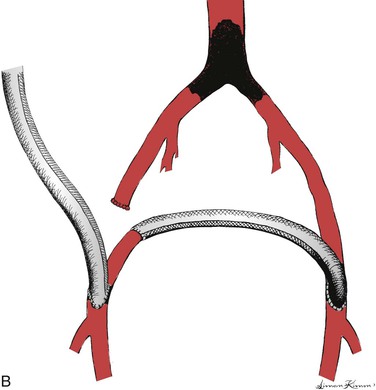
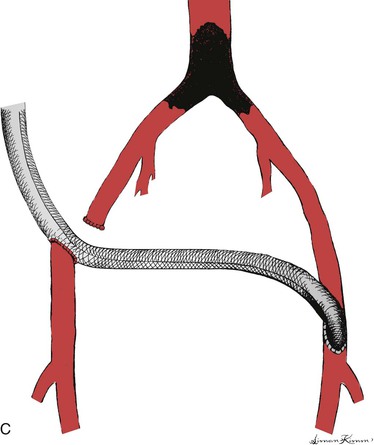
Figure 111-3 Three configurations of axillobifemoral bypass grafts. All three are shown with a right-sided axillofemoral graft component. A, The most common configuration.81 B and C, Modifications described by Blaisdell22,232 and Rutherford et al,233 respectively, designed to prevent competitive inflow from a patent ipsilateral iliac system.22
Results
Effects of Surgical Indications and Patient Characteristics on Results
Early Literature.
Earlier series of axillofemoral bypasses made it clear that axillofemoral bypass provided acceptable patencies in high-risk patients212–214,236 but the emergence and adoption of life-table methods for patency estimates allowed more meaningful comparisons between axillofemoral bypass and aortofemoral bypass and between series of axillofemoral bypass. Examination of reports of axillofemoral bypass yields perhaps the broadest range of long-term patencies of any arterial reconstructive procedure.101,237 A prior review of pertinent articles regarding axillofemoral bypass and confined primarily to patients with chronic lower extremity arterial occlusive disease published between 1960 and 1993 yielded 3-year primary patency estimates as low as 39% and as high as 85%.238 A subsequent 1996 report from Passman et al reported 5-year estimated primary patency of 74%.239
There are many potential explanations for these discrepancies. Patients undergoing axillofemoral bypass as part of the treatment for infection of the aorta or an aortic prosthesis or for aortoenteric fistula tend to suffer high perioperative morbidity and mortality, but with respect to graft patency and limb salvage results have varied. Oblath et al240 and Hennes et al199 reported generally mediocre results, but other investigators report that survivors are likely to enjoy better patency than those with chronic severe arterial occlusive disease.101,198,241,242 Series including substantial numbers of such patients will generally report a more favorable patency experience. On the other hand, it is likely that patients undergoing emergent axillofemoral bypass for acute lower extremity ischemia suffer substantially more early and late complications than do those undergoing surgery in more elective circumstances.243,244 Results after primary operations, including axillofemoral bypass can be expected to be superior to those for secondary operations.101 Patient characteristics and surgical indications influence outcome and must be considered when reading published reports of results of axillofemoral bypass. Axillofemoral bypass was also initially proposed only for high-risk patients,210,211,215,216 but by the mid- to late-1970s, some authors advocated extending these procedures to more patients and in some cases even advocated axillofemoral bypass as the procedure of choice for all but the youngest and healthiest of patients when anatomy allowed.130 Many surgeons were strongly influenced by three specific favorable reports,81,245,246 but the favorable experience reported in these articles may have been due to the characteristics of the patients reported and the approach to patency reporting.
Claudication versus Critical Limb Ischemia.
Claudicants have generally been found to enjoy better patency than patients with CLI for virtually every type of arterial reconstruction for chronic lower extremity arterial disease (with the possible exception of femorofemoral bypass, see earlier). Furthermore, claudicants tend to live longer than patients with CLI and through that mechanism tend to contribute to patency life tables longer than do those with CLI. Thus series with substantial numbers of low-risk claudicants tend to report disproportionately favorable patency experience than do those restricted to high-risk patients with CLI.247 If analysis is confined to high-risk patients, then most patients are likely to suffer from critical limb ischemia, patency is likely to be poorer, and late mortality is likely to be high. These issues and considerations have probably not changed significantly over time. For example, Bliss and Barrett reported estimated survival of only 43% at 28 months after axillofemoral bypass,214 Devolfe et al observed an approximately 35% 3-year survival 10 years after Bliss,219 and we reported 35% 3-year estimated survival 20 years after Bliss.93 However, as longevity of patients with cardiac and other comorbid diseases has improved over the last several years, the survival of patients undergoing axillofemoral bypass may also have improved. Huded et al reported 5-year survival of more than 40% in the most recent substantial study including axillofemoral bypass patients.108
Secondary Patency.
Finally, some of these favorable reports were based on the use of what is currently termed “secondary patency.” Nearly all authors have noted that axillofemoral bypass grafts are more likely than aortofemoral grafts to thrombose, and the favorable secondary patency of the former was at the expense of a significantly more frequent requirement for graft thrombectomy. Some reports have also considered the axillofemoral and femorofemoral components of axillobifemoral grafts as two distinct grafts, thus doubling the total number of “observed” grafts. Using this approach, thrombosis of one component has only half as much impact on the patency calculations as it would if the entire graft is considered as a unit. We consider this approach to be misleading since patients would find little consolation in persistent patency of half of their graft when told they will require amputation because of thrombosis of the other component of their graft.
Systematic Review.
Review of the published literature addressing axillofemoral bypass for chronic lower extremity ischemia since those earlier favorable reports has generally been much less optimistic. Two exceptions have been the favorable experience of Ray et al and El-Massry et al from the same group in Seattle and reports from the group at the Oregon Health Sciences University.81,239,248,249 It is instructive to examine these reports after stratification by operative indication. For example, Corbett et al reported 38% secondary patency at 2 years in a series composed of only patients with CLI,250 whereas Ray et al (roughly contemporary with Corbett et al and including 59% claudicants) reported 79% primary patency at 3 years. Dé and Hepp had to perform at least 1 and as many as 5 explorations for thrombosis in half of 131 axillofemoral bypass grafts.251 KA Harris et al reported only a 53% 3-year patency,252 whereas EJ Harris et al reported 78% 5-year primary patency in roughly the same era.248 Urayama et al noted markedly reduced primary patency for extra-anatomic bypass compared with direct aortofemoral reconstruction, but the former group was older, more likely to have critical limb ischemia, and had markedly lower survival to at least 10 years after the procedure.253
Table 111-2 represents a review including reports that appeared to adhere to current reporting standards.* We selected articles that we thought provided adequate information about indications for axillofemoral bypass, comorbidities, and late mortality; clearly used life-table methods to calculate patency as defined using Society for Vascular Surgery criteria261,262; and when possible, included data only from patients with chronic or acute arterial occlusive disease, excluding data related to arterial or prosthetic graft infection. It was unclear in some of these articles whether patency was calculated by number of graft limbs or number of patients. These studies are arranged in Table 111-2 in order of ascending primary patency. Only two primary reports of axillofemoral bypass that I could identify published in the last 20 years appear to qualify for inclusion in Table 111-2 based on the just-described criteria, although there does seem to be a trend toward lower operative mortality in some more recent reports that are not included in Table 111-2.263–266 With the exception of the report of Donaldson et al,257 the results of the reports included in Table 111-2 are fairly easily separated into series with few claudicants, including our own previous report and series that include significant numbers of claudicants, the former comprising seven of the first eight citations and the latter consisting of Donaldson et al, plus the last five citations in the table. Thus it appears that inclusion of as few as 20% claudicants in such a series has a potentially dramatic impact on the patency experience of axillofemoral bypass. Operative and late mortality, where reported, are also lower in those series with larger numbers of claudicants, thus enhancing the patency predictions by the mechanisms discussed earlier. Finally, a wide range exists in the frequencies of various comorbidities in patients undergoing axillofemoral bypass, reinforcing the contention that the definition of “high-risk” differs among institutions. Jämsén et al and Huded et al have provided an excellent description of their results, but these reports did not clearly distinguish claudicants from those with CLI to an adequate extent to allow inclusion in Table 111-2.108,263 However, review of those authors’ results show them to be generally consistent with those described by others and included in Table 111-2, except for improving mortality as noted earlier.
Table 111-2
Comparison of Indications, Patient Characteristics, and Mortality with Axillofemoral Graft Patency
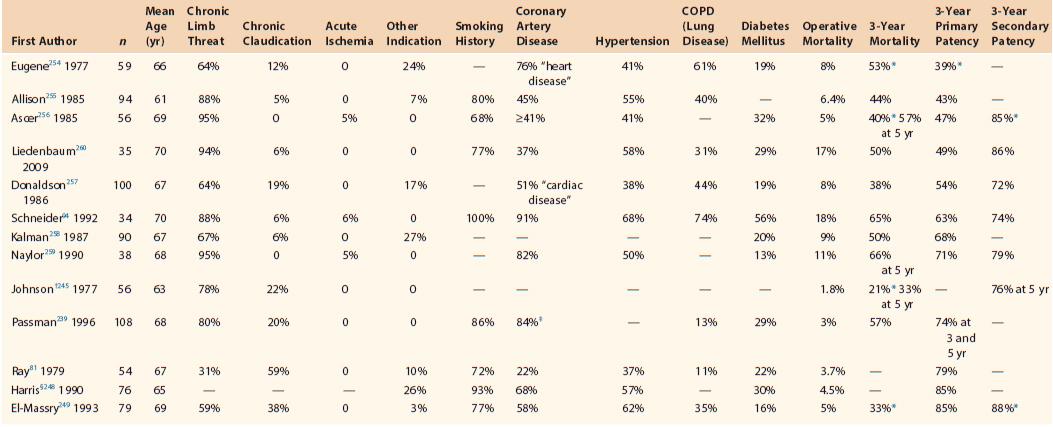
* Not quoted for 3 years but estimated from life table graphs in original article.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


