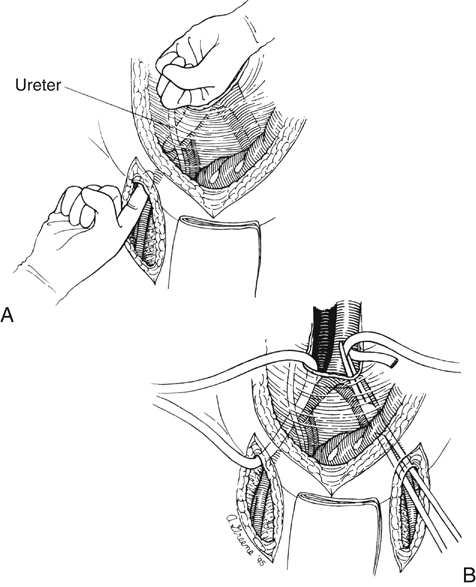
After the aortic and femoral artery dissection are completed, retroperitoneal tunnels between the two fields of dissection are made for subsequent passage of each graft limb. Such tunnels are best made by gentle blunt dissection with the index finger of each hand simultaneously from the groins and the area of the aortic bifurcation (Figure 1). Dissection should be kept on a plane directly anterior to the common and external iliac vessels to ensure that the graft is subsequently placed posterior to the ureter. This detail is important because passage of graft anterior to the ureter can lead to later compression and obstruction of the ureter and hydronephrosis. After appropriate tunnels have been created to both groins, a long blunt-tipped clamp is placed through the tunnel, and a Penrose drain is drawn through the tunnel. Elevation on both ends of this facilitates later passage of the graft limbs to the site of distal graft anastomosis.
Aortofemoral Bypass for Atherosclerotic Aortoiliac Occlusive Disease
Operative Management
Tunnel Construction
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Aortofemoral Bypass for Atherosclerotic Aortoiliac Occlusive Disease
