11 Aorto-Ostial and Branch Ostial Lesions and Unprotected Left Main Percutaneous Coronary Interventions 
Techniques for Ostial PCI
Balloon Catheter Placement
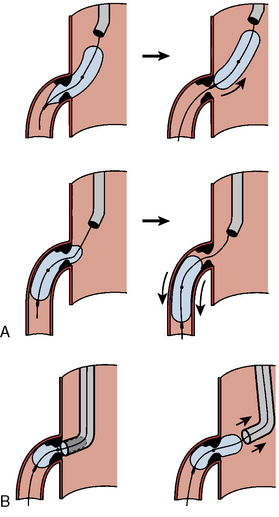
Balloon angioplasty requires seating such that, during inflation, the balloon will not be ejected from, nor compressed forward past (“watermelon seed”), the coronary ostia (Fig. 11-1). Removal of the guide catheter into the aorta immediately before balloon inflation will permit the balloon to be inflated partly in the coronary ostium and the aorta and outside the guide catheter. The lesion will be appropriately spanned by the two ends of the balloon inflating at equal pressure. Inflation in the guide may result in failure of the distal end of the balloon to inflate properly. Stenting the ostial lesion may produce strut “hangout” into the main vessel, a common complication of ostial branch stenting, especially when angiographic angles do not allow good visualization of the takeoff. An anchor wire technique may obviate this problem.
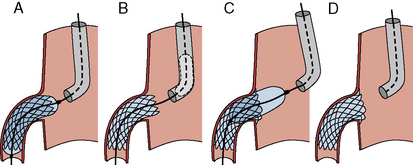
Figure 11-2 demonstrates good techniques for RCA ostial stenting. Recovering access to the main vessel after ostial stenting can be difficult depending on the angle of the ostium origin and the amount of stent. It may be helpful to leave the stent balloon catheter in place and advance the guide catheter over the balloon to minimize damage or disfiguration of the recently implanted stent.
The Back-Stop Technique
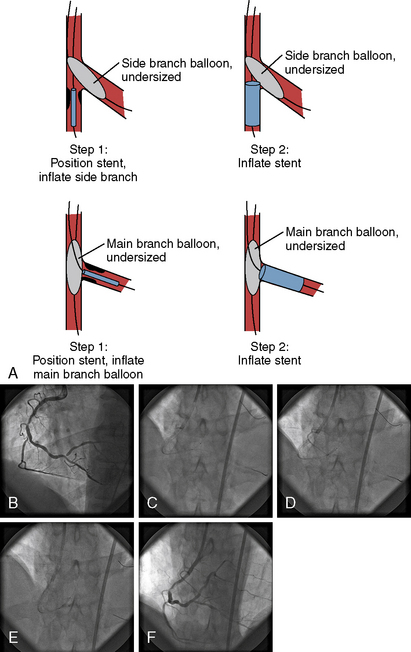
A strategy to prevent strut hangout uses a main vessel balloon inflated at low pressure (balloon:artery ratio 0.7:1), placed prior to branch stent deployment (Fig. 11-3). By pulling the ostial stent back against the inflated balloon and then deploying the stent, one prevents significant strut hangout into the main vessel.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree