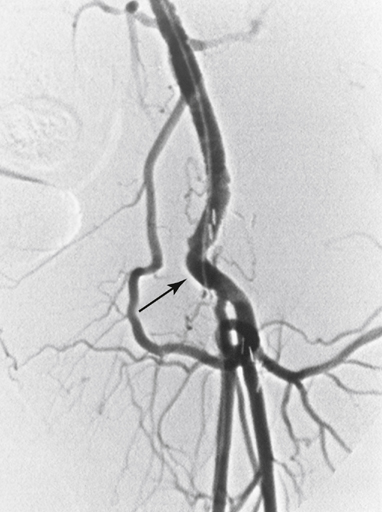
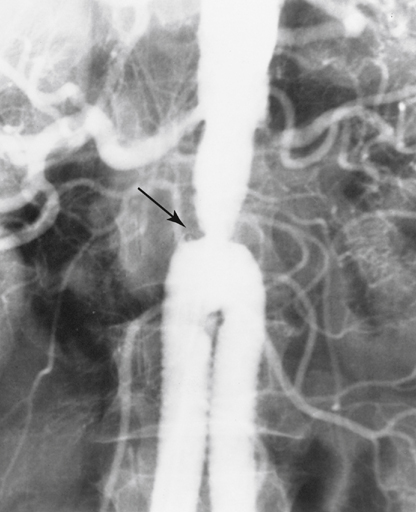
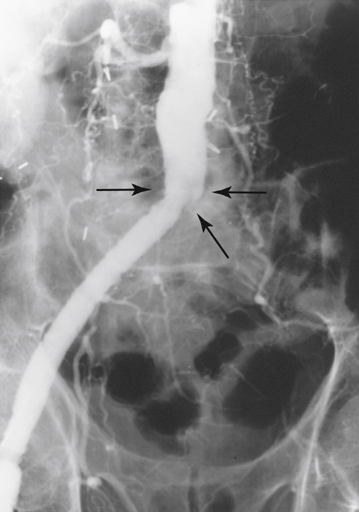
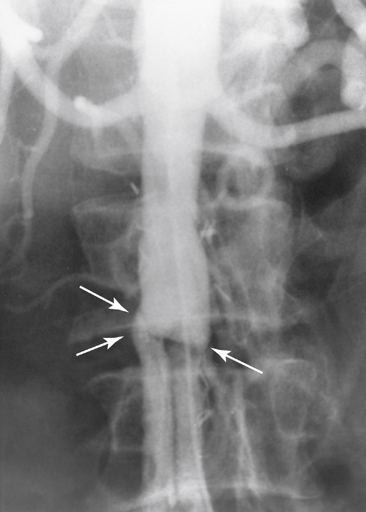
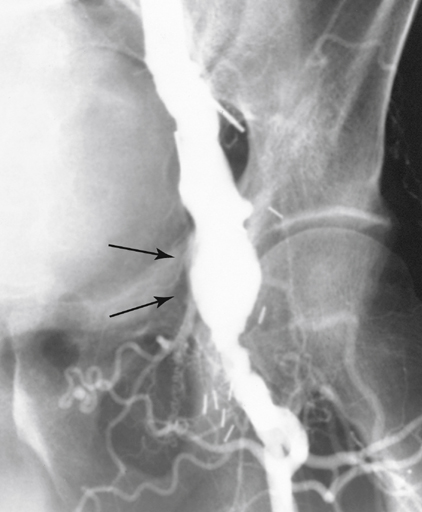
Causes of aortic graft limb occlusion can be best conceptualized as early or late. Early postoperative thrombosis of an AFB graft limb most commonly results from a technical problem. Such problems most often occur with either the handling of the graft or the construction of the distal anastomosis at the time of AFB graft placement. Generally, inflow from the aorta is not a problem, provided that a major clamp injury or dissection has not occurred. Correct handling of the graft includes its proper placement without twisting through the retroperitoneal tunnel to the femoral position. Proper graft length is critical because redundant graft near either anastomosis tends to kink and obstruct blood flow (Figures 1 and 2). Extended graft body versus limb length can also cause a kink at the origin of the limb as it traverses the pelvis to the inguinal ligament. Proper technical execution of the distal anastomosis requires careful clamping of an often diseased superficial femoral artery (SFA) or profunda femoral artery (PFA) to avoid creating intimal flaps. Adequate intraprocedural anticoagulation and ample flushing of the graft and vessels of air or thrombus that have accumulated in the graft during construction of the anastomoses is also important. Late thrombosis of an AFB limb generally occurs secondary to progressive intimal hyperplasia or progression of outflow atherosclerotic disease at the distal anastomosis. In the first few years after graft placement, luminal narrowing can result from intimal hyperplasia from a clamp injury or turbulent flow from a large-diameter prosthetic graft anastomosed to diminutive artery. Late thrombosis results primarily from progression of distal arteriosclerotic disease. This may also be associated with an anastomotic aneurysm (Figure 3). The anastomotic aneurysm, upon enlarging, develops luminal thrombus, resulting in a thrombogenic milieu that can precipitate graft limb occlusion. Rarely, a proximal aortic stenosis occurs and leads to aortic graft limb thrombosis (Figure 4). This condition is best avoided by placing the proximal graft-to-aorta anastomosis as close as possible to the origins of the renal arteries. Certain important anatomic information, usually evident on computed tomography arteriography (CTA), is very helpful for determining the optimal treatment options. The aortic anastomosis must be visualized to determine whether there is adequate inflow to the graft, the presence of thrombus in the body of the graft or the contralateral limb, or the suggestion of an aortic anastomotic aneurysm (Figures 5 and 6). It is also important to visualize the contralateral limb to determine whether intrinsic graft degeneration may be occurring, although it is unusual in grafts today. In some instances, there is poor visualization of the reconstituted vessels on the affected side of the occluded graft limb as a result of poor collateral filling with CT contrast bolus. Poor or nonvisualization of the reconstituted vessels should not discourage attempted reconstruction because patent vessels may be identified with intraoperative arteriography at the time of surgery. In fact, direct opacification of the PFA provides better identification of distal runoff vessels should a distal bypass be necessary.
Aortic Graft Limb Occlusion
Etiology
Management
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Thoracic Key
Fastest Thoracic Insight Engine