Aortic Arch Debranching
JIP L. TOLENAAR, GIANBATTISTA TSHIOMBO, and SANTI TRIMARCHI
Presentation
An 84-year-old female presents to the outpatient ENT clinic with complaints of dysphonia. Direct laryngoscopy shows paralyses of the left vocal cord. A CT scan was obtained to help determine the cause of the vocal cord paralysis (Fig. 1). The patient is referred to you after a diagnosis of a saccular aortic arch aneurysm, 6 cm in diameter, was detected by CTA. On physical examination, a questionable pulsatile abdominal mass is noted. The patient is noted to have normal femoral/popliteal/pedal pulses bilaterally.
Differential Diagnosis
This patient has an extensive and complicated aortic arch aneurysm causing dysphonia. While most of these aneurysms are repaired in good-risk patients using circulatory arrest, a hybrid procedure using aortic arch and stent grafting is preferred in high-risk patients. Typically, this can be performed in either a one- or two-step procedure. Besides degenerative aortic aneurysms, postdissecting aneurysms are a common late complication of a persistent false lumen after type A aortic dissection and some medically treated type B aortic dissections.
Workup
All patients with aortic arch aneurysms should have a CT scan with intravenous agent from the carotid to the femoral arteries. The present patient’s CTA (Fig. 1) documents a thoracic aortic arch aneurysm with no abnormalities of the supraaortic brachiocephalic arteries. The use of 3D reconstructions provide a great opportunity to study the morphology of the pathology and to determine whether a direct surgical approach or a hybrid approach with a stent graft and debranching procedure is preferred. Echocardiography showed an ejection fraction of approximately 60%, a cardiac catheterization revealed no significant coronary disease, and her pulmonary function tests are acceptable.
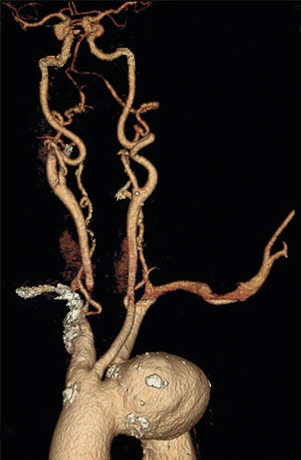
FIGURE 1 Preoperative CT scan showing saccular aortic arch aneurysm.
Discussion
Isolated aortic arch disease is relatively uncommon and is usually part of multilevel aortic disease. Treatment of aortic arch disease is challenging and associated with considerable morbidity and mortality, especially in patients older than 75 years of age. A recent large series of open aortic arch repairs reported an early mortality between 4% and 13%, a stroke rate between 1.6% and 9.2%, and spinal cord ischemia ranging from 0% to 13%.
Diagnosis and Treatment
The treatment of aortic arch disease is challenging and associated with considerable morbidity and mortality. The use of selective cerebral perfusion and hypothermic circulatory arrest for brain protection during open surgery for aortic arch disease has considerably improved outcomes, although mortality and morbidity remain substantial. Because of the anatomy of the aortic arch with its side branches, a standard endovascular approach is not yet available in these patients. Therefore, a hybrid approach, which combines debranching of supraaortic arteries with stent graft placement in the thoracic aorta, has become an attractive alternative for high-risk patients. Based on the intended proximal landing zone (LZ) of the stent graft, patients are classified according to the Ishimaru classification. In patients with LZ0, the ascending aorta is used as the proximal LZ and the innominate artery (IA) is covered, requiring revascularization of all supraaortic brachiocephalic branches through a median sternotomy or through extra-anatomic debranching. In case of LZ1, the left common carotid artery (LCCA) and left subclavian artery (LSA) are covered and an extra-anatomic carotid-carotid bypass and revascularization of the left LSA is needed. When only the LSA is covered (LZ2), a left subclavian bypass or transposition is recommended, as this decreases the incidence of spinal cord ischemia and stroke.
Surgical Approach for Thoracic Aortic Arch Debranching
The procedure is performed under general anesthesia, and cerebral monitoring is used throughout the entire procedure. The patient is prepped from head to knees and draped in sterile fashion. A medium sternotomy is performed, and the pericardium is opened. After heparinization, the ascending aorta is tangentially clamped. With the use of a reversed aortobifemoral prosthesis, an end-to-side anastomosis is made between the graft and the ascending aorta. Subsequently, the IA is transected, and after the origin of the IA is clamped and ligated, an end-to-end anastomosis is performed to the graft. Subsequently, the other limb is used to perform an end-to-end anastomosis with the LSA. Depending on the anatomy, the graft is preferably placed deep to the innominate vein, to avoid compression of the vein. Finally, the left common carotid artery is reimplanted in the limb of the prosthesis in an end-to-side fashion. Closure of the chest is performed with sternal wires and the soft tissue closed in multiple layers. The second stage of the procedure, which can be performed in the same setting or during a second procedure, consists of placement of two stent grafts, covering all ligated branches. Postdeployment angiography demonstrated appropriate placement of the stent grafts with aneurysm exclusion and no endoleaks. After all catheters and wires are straightened and removed, an Angio-Seal device is deployed in one groin, and the arteriotomy in the femoral artery is closed. A postoperative CTA showed adequate exclusion of the aneurysm (Fig. 2; Table 1).

FIGURE 2 Postoperative CT scan showing total aortic arch debranching and aneurysm exclusion using TEVAR.



