Aorta
Craig R. Asher • Gian M. Novaro
QUESTIONS
Case 1 (Questions 1 to 3)
A 78-year-old woman is referred to cardiology clinic for management of aortic regurgitation. The patient has no cardiac risk factors except mild hypertension (HTN) on monotherapy and has not previously undergone cardiac testing. A review of systems is notable for recent onset of headaches and myalgias.
Physical Examination
Blood pressure (BP)—138/78 mmHg in both arms; pulse—62 bpm.
Funduscopic examination reveals no changes consistent with hypertensive retinopathy. The heart examination is notable for a normal S1 and increased intensity S2 (A2). An S4 gallop, II/VI diastolic decrescendo murmur heard best at the right sternal border, and III/VI early-peaking systolic ejection murmur heard at the left sternal border are present. There is no systolic ejection click. The carotid pulse is of normal intensity and contour and the pulses in the upper and lower extremities are strong and equal.
Electrocardiogram (ECG) reveals sinus rhythm with nonspecific ST changes.
1.What is the most likely explanation for the patient’s heart murmur?
a.Bicuspid aortic valve with severe aortic regurgitation
b.Bicuspid aortic valve with severe aortic stenosis and moderate aortic regurgitation
c.Degenerative severe aortic valve stenosis and moderate aortic regurgitation
d.Aortic dilatation with moderate aortic regurgitation and mild aortic stenosis
A transthoracic echocardiogram (TTE) is performed showing normal left ventricular (LV) size and function with a trileaflet aortic valve. Aortic measurements are as follows: sinus of Valsalva—4.0 cm; sinotubular junction—4.4 cm; mid-ascending aorta—4.5 cm with moderate effacement of the sinotubular junction. Peak and mean aortic gradients are 22/13 mmHg with moderate (2+) aortic regurgitation. A small circumferential pericardial effusion is present. Laboratory tests reveal an erythrocyte sedimentation rate of 74.
2.What additional test would be most helpful in determining the etiology of the patient’s aortic dilatation and aortic regurgitation?
a.Coronary angiogram and aortography
b.Magnetic resonance angiography (MRA) of the great vessels
c.Computed tomographic angiography (CTA) of the ascending aorta
d.Transesophageal echocardiography (TEE)
3.What is the most likely diagnosis to explain the patient’s aortic dilatation and aortic regurgitation? See Figure 6.1.
a.Takayasu arteritis
b.Degenerative aortic disease
c.Connective tissue disorder
d.Giant cell arteritis
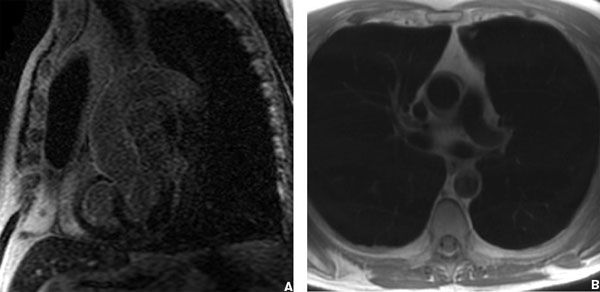
Figure 6.1
Case 2 (Questions 4 to 6)
An 18-year-old woman presents for her annual physical examination. She had a brother with Marfan syndrome who was 24 years old when he died suddenly. She is active and asymptomatic.
Physical Examination
5 feet 7 inches (170 cm) and 150 pounds (68 kg).
Arm span-to-height ratio = 1.07.
Head and neck examination is notable for a high-arched palate and a slit-lamp examination shows ectopia lentis. Musculoskeletal examination is notable for a pectus carinatum and positive wrist and thumb sign. Cardiac examination is notable for a mitral valve click and a soft murmur of mitral regurgitation.
4.What additional testing is needed to determine whether this young woman has Marfan syndrome?
a.TTE
b.Genetic testing
c.CT angiogram of the aorta
d.No additional testing
A TTE is performed that shows mitral valve prolapse with mild (1+) mitral regurgitation. The aortic root is dilated at 5.0 cm with effacement of the sinotubular junction and a mid-ascending aortic measurement of 3.6 cm. The aortic valve is trileaflet with no aortic regurgitation.
5.What is the most important recommendation to be made to this patient?
a.Repeat the TTE in 6 months
b.Initiate a β-blocker
c.Avoid strenuous exertion, contact sports, and pregnancy
d.Elective aortic replacement
The patient wishes to schedule surgery but prefers to wait 2 months until the end of the school year. Her father who is an internal medicine physician has read about the potential benefit of angiotensin receptor blockers (ARBs) for patients with aneurysms and asks your advice regarding treatment.
6.What is the postulated mechanism of action whereby ARBs reduce progression of aortic disease in Marfan syndrome?
a.Reduction of BP through angiotensin II type 1 receptor blockade
b.Complete blockade of the renin–angiotensin–aldosterone system
c.Reduction in activity of transforming growth factor (TGF)-β
d.Increase production of matrix metalloproteinases (MMPs)
Case 3 (Questions 7 and 8)
A 67-year-old man with long-standing HTN presents to the emergency room (ER) with sudden-onset chest pain described as ripping in quality, subsiding since its onset. He underwent a cardiac catheterization 6 months previously that showed a 40% lesion in the mid-left anterior descending coronary artery. His medications include aspirin, gemfibrozil, and nifedipine.
Physical Examination
He appears diaphoretic. HR—110 bpm; BP—106/54 mmHg (right arm); 72/35 mmHg (left arm). Jugular venous pressure—12 cm H2O. Heart sounds are soft and there is no audible systolic or diastolic murmur. Left radial and brachial pulses are weak.
ECG on presentation shows ST elevations in the inferior leads and low voltage.
Chest X-ray (CXR) shows cardiomegaly with a globular-shaped heart and interstitial edema.
7.Which of the following is the first diagnostic test that should be performed?
a.Cardiac enzymes
b.MRA of the aorta
c.TTE
d.Cardiac catheterization
A TTE was performed showing a pericardial effusion and signs of cardiac tamponade. A CT angiogram is also performed and shown in Figure 6.2.
8.What intervention should be performed next for the management of this patient?
a.Cardiac catheterization
b.Emergent aortic surgery
c.Swan-Ganz catheterization
d.Pericardiocentesis
Case 4 (Questions 9 and 10)
A 36-year-old man with a bicuspid aortic valve develops sudden onset of headache, mental status changes, and unequal pupils. He is rushed to an ER and a head CT scan is done that shows an intracranial bleed. BP on presentation is 158/78 mmHg.

Figure 6.2
Except for a history of HTN, he has no known medical problems and no history of drug abuse. A visit to his physician’s office 1 week earlier revealed a BP of 120/75 mmHg on metoprolol and ramipril.
9.What is the most likely reason for the patient’s intracranial bleed?
a.Hypertensive crisis
b.Aortic dissection
c.Cerebral aneurysm rupture
d.Mycotic aneurysm associated with endocarditis
10.What other structural abnormality is most commonly associated with coarctation of the aorta?
a.Atrial septal defect
b.Ventricular septal defect
c.Pulmonary stenosis
d.Mitral valve prolapse
Case 5 (Questions 11 and 12)
A 74-year-old man presents to the ER with upper back pain ongoing for 3 hours. The pain is described as sharp and severe occurring at rest. He has no associated symptoms of shortness of breath, chest pain, or presyncope. His past medical history is notable for a coronary artery bypass graft (CABG) 2 years previously, HTN, and ongoing tobacco use. At the time of his CABG, he was noted to have a 4.4-cm ascending aortic aneurysm that was not repaired. His medications include aspirin, an angiotensin-converting enzyme inhibitor, and a β-blocker.
Physical Examination
BP—180/110 mmHg.
Pulse rate—90 bpm.
Lung and cardiac examinations are unremarkable and no cardiac murmur is heard. The abdomen is mildly tender with no bruit. Pulses are equal but diminished in the lower extremities.
ECG shows sinus rhythm with nonspecific ST changes and an old inferior myocardial infarction (MI).
Laboratory tests including cardiac enzymes, liver function tests, amylase, and lipase are normal.
11.What is the most appropriate diagnostic procedure to perform next?
a.TTE
b.TEE
c.CTA of the chest and abdomen
d.Aortography
A CT scan demonstrates an ascending aortic aneurysm of 4.8 cm and a descending thoracic aortic aneurysm of 6.0 cm but no evidence of dissection. There is no abdominal aortic aneurysm (AAA). The patient continues to have ongoing pain despite high doses of β-blockers, sodium nitroprusside, and opioid analgesics.
ECG and cardiac enzymes remain normal.
D-dimer level is >500 ng/mL.
12.What is the most appropriate next decision for management?
a.Cardiac catheterization
b.MRA of the chest/aorta
c.TEE
d.Intensify medical therapy
Case 6 (Question 13)
A 62-year-old man presents for a routine annual examination. He has a history of HTN that is managed with monotherapy. He is active and has no symptoms.
Physical Examination
BP—162/88 mmHg in both arms. Pulse rate—70 bpm. Heart and lung examination is unremarkable. Abdominal examination reveals a pulsatile mass.
ECG shows sinus rhythm and a complete right bundle branch block.
Abdominal ultrasound shows an infrarenal AAA of 4.2 cm.
13.What is the most appropriate management step?
a.Initiate a β-blocker and repeat ultrasound in 6 months
b.Initiate a β-blocker and repeat ultrasound in 3 months
c.No medical therapy and repeat ultrasound in 1 year
d.No medical therapy and repeat ultrasound in 2 years
Case 7 (Questions 14 and 15)
A 76-year-old man presents to the ER with severe sharp chest pain that began 2 hours previously. He has a history of HTN and had CABG 3 years ago after an MI. He continues to smoke. The CABG was performed off-pump because of severe atheroma in the ascending aorta seen by intraoperative TEE. The patient’s pain has not subsided with the initiation of IV heparin, nitroglycerin, and β-blockers. The pain is different in character from the pain before his MI.
Physical Examination
BP—160/94 mmHg.
Pulse—76 bpm.
Heart and lung sounds are normal. Pulses are diminished in the lower extremities.
ECG shows a left bundle branch block.
Cardiac enzymes are normal × 1.
Despite severe atheroma in the aorta, the physician taking care of the patient is not convinced that he does not have an acute coronary syndrome and performs a cardiac catheterization. It shows that the grafts are patent and there is no culprit lesion in the native vessels. He then decides to perform aortography and a focal outpouching is seen in the aortic wall in the distal ascending aorta (Fig. 6.3A). Contrast dye collects slowly in this region. The patient’s chest pain is intensifying. A TEE is also performed (Fig. 6.3B).
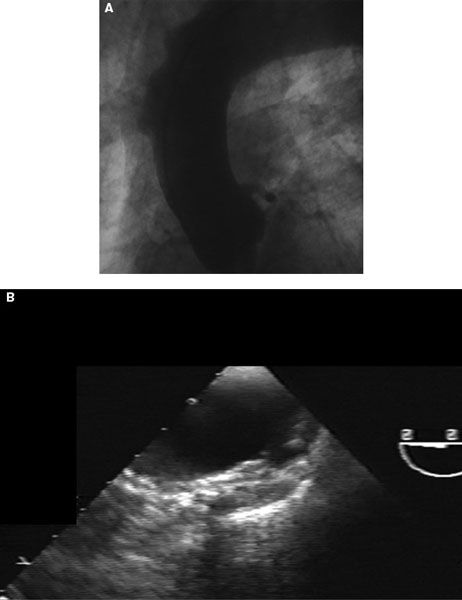
Figure 6.3
14.What is the correct diagnosis?
a.Aortic dissection
b.Aortic aneurysm
c.Intramural hematoma
d.Penetrating aortic ulcer
15.What is the most appropriate next management step to take?
a.Medical management with β-blockers and afterload reduction
b.Transfer to the operating room immediately for replacement of the ascending aorta
c.Medical management and obtain a CT chest/aorta
d.Medical management and obtain an MRA of the aorta
Case 8 (Questions 16 and 17)
A 45-year-old woman presents with discomfort in her left leg with walking, dizziness, headaches, and a cold right hand. She has no chest pain or shortness of breath. There is no significant past medical history and she does not smoke.
Physical Examination
BP—170/82 mmHg (left arm) and 140/68 mmHg (right arm). Lung sounds are clear. Cardiac examination is notable for a normal S1 and S2 and II/VI diastolic decrescendo murmur at the left sternal border. The right brachial pulse is diminished and lower extremity pulses are diminished. A bruit is heard over the left carotid artery and right subclavian artery.
16.What test would be most useful for diagnosing the patient’s condition?
a.TEE
b.Carotid duplex ultrasound
c.Magnetic resonance imaging (MRI) of the head
d.Angiography
17.What is the most likely diagnosis?
a.Behçet disease
b.Relapsing polychondritis
c.Giant cell arteritis
d.Takayasu arteritis
Case 9 (Questions 18 to 21)
A 21-year-old woman with Turner syndrome has a history of surgical repair for periductal coarctation of the aorta at age 4 years. Her presentation was for HTN and heart failure, both of which resolved after the procedure. She was lost to follow-up after childhood and recently reestablished with a cardiologist. She has been experiencing dyspnea and claudication in the past year.
Physical Examination
BP—188/94 mmHg (left arm); 192/100 mmHg (right arm); 100/60 mmHg (right leg).
Pulses are notable for normal upper extremity and reduced lower extremity pulses with a brachial–femoral delay. Cardiac examination is notable for normal S1 and paradoxically split S2 with an ejection click and S4 gallop. A continuous murmur III/VI in intensity is heard under the left scapula.
18.Which of the following statements is correct regarding the echocardiographic image from this patient obtained from the suprasternal notch (Fig. 6.4)?
a.Pressure gradients are usually underestimated using the simplified Bernoulli equation
b.Pressure gradients are usually accurate using the simplified Bernoulli equation
c.Pressure gradients shown are not consistent with severe coarctation
d.Presence of systolic and diastolic flow is consistent with severe coarctation
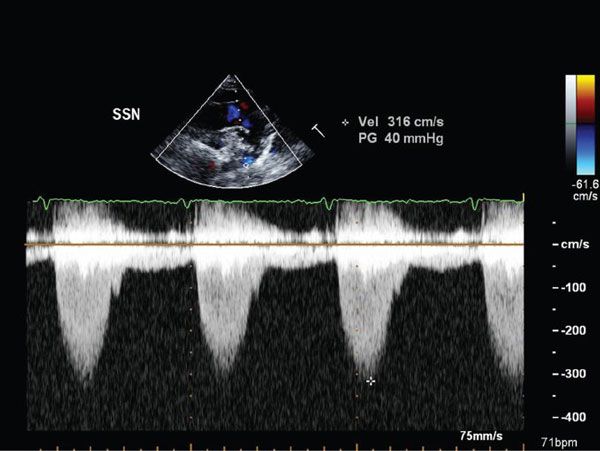
Figure 6.4
19.Which of the following statements is correct regarding the echocardiographic image from this patient obtained from the abdominal aorta (Fig. 6.5)?
a.The hallmark of coarctation is the presence of low systolic velocities
b.The presence of coarctation cannot be determined without knowing the timing of the pulse delay relative to aortic ejection
c.The hallmark of coarctation is the presence of persistent antegrade flow in diastole
d.The presence of coarctation cannot be determined without additional Doppler images proximal to the coarctation site
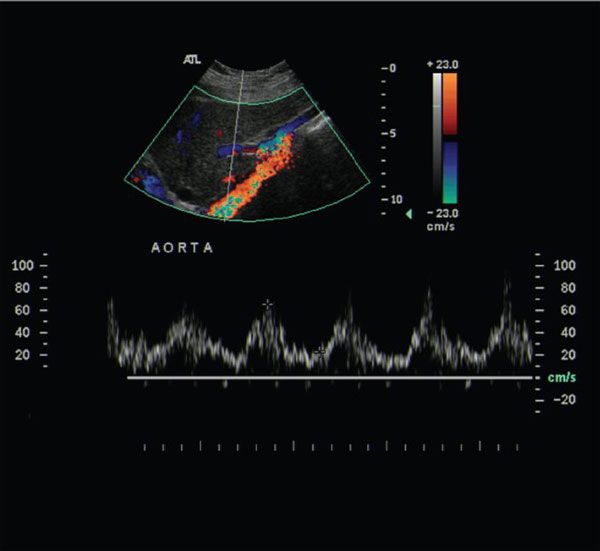
Figure 6.5
20.Which of the following recommendations is most appropriate regarding reintervention in this patient (Fig. 6.6)?
a.Surgery is generally recommended
b.No intervention should be performed until maximal medical therapy is attempted
c.Balloon angioplasty with or without stents is generally recommended
d.There is no consensus and either surgery or balloon aortoplasty (with or without stenting) are equal options

Figure 6.6
21.Which of the following is an indication for aortic coarctation intervention?
a.Symptomatic patient with dyspnea at rest, regardless of the coarctation gradient
b.Asymptomatic patient with normal BP at rest and with exercise and a peak-to-peak gradient across the coarctation site of 19 mmHg
c.Asymptomatic patient with a peak-to-peak gradient across the coarctation site of 15 mmHg with extensive collaterals
d.Symptomatic patient with a bicuspid aortic valve and severe aortic regurgitation undergoing aortic valve replacement and a peak-to-peak gradient across the coarctation of 15 mmHg
Case 10 (Question 22)
A 30-year-old man is referred to cardiology clinic for evaluation of a heart murmur. He had an uneventful childhood except that on four separate occasions he fractured his arms or legs requiring multiple surgical repairs. He has no family history of heart disease or congenital abnormalities.
Physical Examination
Normal stature. Vital signs are normal. Arm span-to-height ratio is normal.
No pectus deformity, scoliosis, wrist sign. Cardiac examination is notable for a decreased S1 and normal S2 intensity with a III/VI diastolic decrescendo murmur and no gallops. Pulses are normal and the extremities are hypermobile. No abnormality of the skin is present.
TTE shows a dilated sinus of Valsalva of 4.7 cm with severe aortic regurgitation. Left ventricular ejection fraction (LVEF) = 65% with LV dimensions of (diastole 6.4 cm; systole 5.1 cm).
22.What is the most likely diagnosis for this patient?
a.Ehlers-Danlos syndrome
b.Marfan syndrome
c.Osteogenesis imperfecta
d.Homocystinuria
Case 11 (Questions 23 and 24)
A 65-year-old man presents to the ER with severe, tearing lower back pain that started while he was shoveling snow. He has a history of poorly controlled HTN and coronary artery disease with a stent to the left anterior descending coronary artery 4 months previously. Other medical problems include severe O2-dependent chronic obstructive pulmonary disease.
Physical Examination
BP—190/110 mmHg.
Pulse—90 bpm.
Cardiac examination is notable for a normal S1 and S2 with an S4 gallop and II/VI early-peaking systolic ejection murmur at the left sternal border.
ECG shows sinus rhythm and no ST changes.
An initial set of cardiac enzymes is normal.
23.What is the most appropriate initial medical therapy?
a.Intravenous metoprolol
b.Intravenous diltiazem
c.Intravenous enalapril
d.Intravenous nitroprusside
A CT angiogram is performed (Fig. 6.7).
24.Which of the following statements regarding the appearance of this form of acute aortic syndrome is most accurate?
a.There is low attenuation of the aortic wall
b.It is not continuous
c.Intimal calcium is nondisplaced
d.It is circumferential or crescentic
Case 12 (Questions 25 to 28)
A 44-year-old man is admitted to the hospital because of a left hemisphere stroke with right arm and leg weakness. He has no history of HTN or smoking, although his total cholesterol level is 334. ECG shows sinus rhythm. Carotid duplex ultrasound shows less than 20% obstruction bilaterally. Head CT demonstrates a recent stroke in the left cortex in the region of the middle cerebral artery. A TTE shows normal valves, chamber sizes, and LV function.
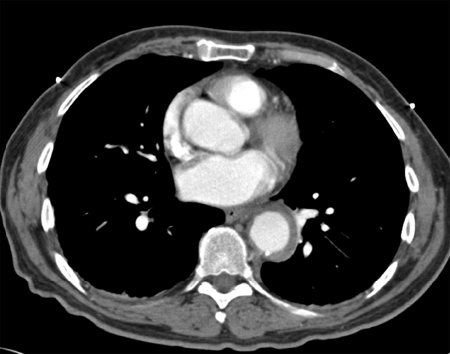
Figure 6.7
25.Which test is most likely to reveal the etiology of the patient’s stroke?
a.TTE with bubble study
b.30-Day event recorder
c.MRA of the head and neck
d.TEE
26.Which of the following medical regimens is most appropriate for a patient with a cardioembolic stroke and the following finding seen on TEE (Fig. 6.8)?
a.Statin and aspirin
b.Statin and warfarin
c.Aspirin and dipyridamole
d.Statin, antiplatelet agent, and warfarin
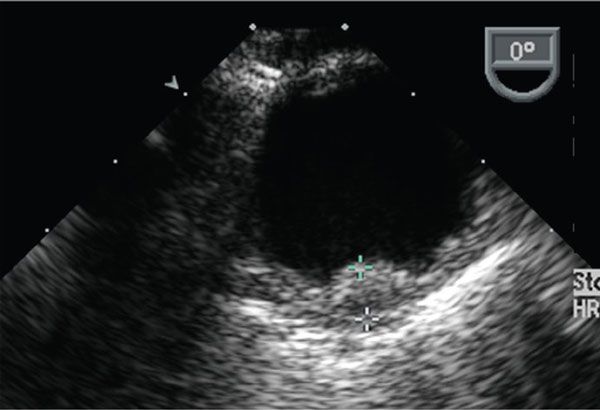
Figure 6.8
27.Which of the following atheromatous plaques is least likely to be associated with a cardioembolic event?
a.3-mm plaque with severe calcification and no mobile components
b.4-mm plaque with small mobile components and no calcification
c.5-mm plaque with multiple mobile components, no calcification, and a small ulceration
d.2-mm plaque with calcification, a small mobile component, and large ulceration
28.Which statement is correct regarding performing CABG in a similar patient with aortic arch atheroma and focal areas of atheroma in the ascending aorta?
a.Palpation of the aorta by the surgeon for calcified plaque correlates with findings of atheroma by TEE.
b.Alternative sites for cross-clamping or cannulation may reduce stroke risk.
c.Aortic arch endarterectomy is recommended.
d.Replacement of the ascending aorta is recommended because of increased likelihood of stroke.
Case 13 (Question 29)
A 21-year-old man is referred to a cardiology clinic for exertional dyspnea. As a child he was evaluated for a heart murmur by a pediatric cardiologist.
Physical Examination
BP—140/84 mmHg (left arm); 120/68 (right arm).
Cardiac examination is notable for a normal S1 and increased intensity S2/A2, absence of an ejection click, and III/VI systolic ejection murmur heard best in the first right intercostal space radiating to the neck and increases with expiration. There is a thrill in the suprasternal notch. The left carotid and brachial pulses are diminished relative to the right carotid and brachial pulses.
29.What diagnosis best explains the patient’s disorder?
a.Patent ductus arteriosus
b.Coarctation of the aorta
c.Supravalvular pulmonary stenosis
d.Williams syndrome
Case 14 (Questions 30 to 32)
A 30-year-old man with a history of congenital heart disease is referred to you because of symptoms of dysphagia and an abnormal CXR. As a child he was told that his CXR was abnormal because of an “aortic anomaly” and that it was benign.
Physical Examination
Vital signs are normal.
Cardiac examination is notable for normal intensity S1 and S2 heart sounds. An ejection click is heard in the right upper sternal border (RUSB) though no murmur is audible. Upper and lower extremity pulses are equal.
30.The CXR (Fig. 6.9) shows what abnormality?
a.Bovine aortic arch
b.Cervical aortic arch
c.Right-sided aortic arch
d.Aberrant right subclavian artery

Figure 6.9
31.What is the most common congenital defect associated with the aortic anomaly seen in Question 30?
a.Tetralogy of Fallot
b.Truncus arteriosus
c.Atrial septal defect
d.Transposition of the great vessels
32.The patient’s dysphagia is likely caused by what abnormality associated with his aortic anomaly?
a.Aberrant left subclavian artery and diverticulum of Kommerell
b.Coarctation of the aorta
c.Isolated aberrant right subclavian artery
d.Interrupted aortic arch
Case 15 (Questions 33 and 34)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


