5 Antithrombotic and Antiplatelet Therapy for Percutaneous Coronary Interventions
Familiarity with commonly used antithrombotic and antiplatelet agents is required in the management of interventional cardiology patients. This chapter outlines recommendations and uses of various antithrombotic and antiplatelet agents. Antithrombotic and antiplatelet agents for percutaneous coronary intervention (PCI) are summarized in Table 5-1, and recommendations from the ACC/AHA are summarized in Table 5-2.
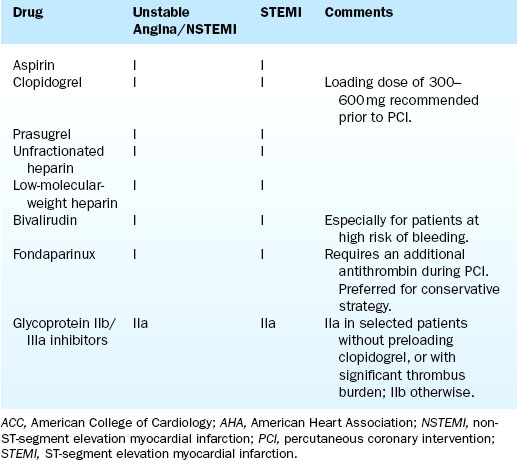
Table 5-1 Antithrombotic and Antiplatelet Agents for PCI Intervention
Table 5-2 ACC/AHA Recommendations for Pharmacologic Management of Patients Undergoing PCI Intervention
Anticoagulants
Heparin
Heparin is given to PCI patients in doses between 40 and 70 U/kg intravenously. Unfractionated heparin (UFH) is a glycosaminoglycan widely used as an anticoagulant. It acts by accelerating the activity of antithrombin III (AT III), a molecule that breaks down the procoagulant factor IIa (thrombin) and factor Xa by forming a complex with AT III and thrombin. Figure 5-1 diagrams the coagulation cascade and role of antithrombins. In contrast, low-molecular-weight heparin (LMWH) is too small to participate in this ternary complex and exerts its effect primarily on factor Xa levels. Both UFH and LMWH are unable to significantly interact with thrombin that is already bound to clot. For this reason adjunctive antiplatelet agents (e.g., aspirin, thienopyridines, and glycoprotein IIb/IIIa receptor antagonists) are typically required for PCI procedures.
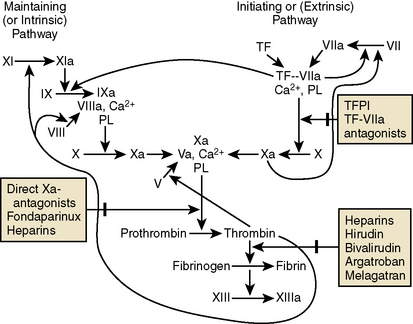
Figure 5-1 Diagrams of the coagulation cascade and role of antithrombins.
(Adapted from Wiley-Liss, Inc., a subsidiary of John Wiley & Sons, Inc. from Conde ID, Kleiman NS. Arterial thrombosis for the interventional cardiologist: from adhesion molecules and coagulation factors to clinical therapeutics. Catheter Cardiovasc Interv 2003;60:236–246.) and Garg R, Uretsky BF, Lev EL. Anti-platelet and anti-thrombotic approaches in patients undergoing percutaneous coronary intervention. Catheter Cardiovasc Interv 2007;70:388–406.
Summary of Heparin Mode of Action
1. Heparin is a mixture of glycosaminoglycans (mucopolysaccharides) that combine with a plasma protein called antithrombin III (AT III) to make the AT III a highly effective inhibitor of thrombin and several other clotting factors.
2. Heparin requires the presence of AT III to be effective.
3. Unfractionated heparin (UFH) is a heterogeneous polysaccharide that binds to antithrombin to inhibit thrombin and factor Xa.
Indications
Side Effects
Heparin-Induced Thrombocytopenia (HIT)
There are two types of heparin-induced thrombocytopenia (HIT) (Table 5-3). Type I HIT (HIT-1) is due to direct (non–immune-mediated) platelet activation, with mild thrombocytopenia and a benign clinical course. Type II HIT (HIT-2) is due to immune-mediated platelet activation, with moderate or severe thrombocytopenia and serious thromboembolic complications. Platelet transfusions should not be used to treat HIT due to increased risk of thrombotic complications. Anticoagulation to prevent thrombosis is the main treatment of HIT-2 patients; typical drugs are the direct-acting thrombin antagonists, lepirudin and argatroban. Compared with UFH, LMWH carries a reduced risk of HIT.
Table 5-3 Heparin-Induced Thrombocytopenia
| Type I Heparin-Induced Thrombocytopenia | Type II Heparin-Induced Thrombocytopenia | |
|---|---|---|
| Incidence | 10% | Rare |
| Mechanism | Direct platelet aggregating effect of heparin | Autoantibody (IgG or IgM) directed against platelet factor IV–heparin complex |
| Onset | Early (1–5 days) | Later (>5 days); may occur sooner if prior heparin exposure |
| Platelet count | 50,000–150,000/mm3 | <50,000/mm3 |
| Duration | Transient; often improves even if heparin is continued | Requires discontinuation of all heparin; gradual recovery in platelet count over 1–5 days in most patients |
| Clinical | Benign | Recalcitrant venous and arterial course thromboses and thromboembolism; may be fatal |
| Heparin | Unfractionated or low-molecular-weight heparin may be continued | Argatroban and lepirudin are FDA-approved |
Modified from Safian R, Grines C, Freed M. The new manual of interventional cardiology. Birmingham, MI: Physicians’ Press, 1999.
Minor Bleeding (Puncture Site, Gums, etc.)
Discontinue heparin. Monitor vital signs, aPTT, hemoglobin, hematocrit, platelet count, ACT.
Use of Heparin as a Bridge to Warfarin Therapy
1. Give heparin 40–70 U/kg IV bolus followed by 1000–1700 U/hr IV infusion.
2. Obtain ACT at 4–6 hr and keep aPTT at 50–90 sec.
3. Start warfarin on day 1 at no more than 10 mg a day.
4. Obtain INR and platelet count.
5. Give heparin and warfarin jointly with heparin for 3 to 5 days, and until INR is between 2.0 and 3.0, then stop heparin.
Low-Molecular-Weight Heparin
LMWHs are fractionated heparins with molecular weights between 3000 and 7000 daltons (UFH is 3000–30,000 daltons). The therapeutic dose of the most commonly used LWMH, enoxaparin, is 1 mg/kg subcutaneously every 12 hours. Patients requiring PCI require additional intravenous bolus doses of enoxaparin to ensure adequate anti-Xa activity for the procedure. Table 5-4 describes suggested doses for PCI.
Table 5-4 Suggested Dosing of Enoxaparin Prior to PCI
| Preprocedure Enoxaparin | IV Bolus Enoxaparin Dose at Time of PCI |
|---|---|
| No prior enoxaparin | 0.75 mg/kg IV |
| Prophylactic doses of enoxaparin only | 0.5 mg/kg IV |
| One-two 1 mg/kg SQ doses, last <8 hrs prior | 0.3 mg/kg IV |
| One-two SQ doses, last 8–12 hrs prior | 0.3–0.5 mg/kg IV |
| Adequate (>3) SQ doses, last <8 hrs prior | No additional enoxaparin |
| Adequate (>3) SQ doses, last 8–12 hrs prior | 0.3 mg/kg IV |
| Any doses, >12 hours | Can use alternative antithrombin |
LMWHs have features distinct from UFH, including:
1. More predictable anticoagulation effect
2. Lack of inhibition by platelet factor 4
3. Lack of need for monitoring
Table 5-5 compares features of LMWHs with UFH.
Table 5-5 Comparison of Low-Molecular-Weight and Unfractionated Heparin
| Characteristic | Unfractionated Heparin | Low-Molecular-Weight Heparin |
|---|---|---|
| Composition | Heterogeneous mix of polysaccharides; molecular weight 3000–30,000 | Homogeneous glycosaminoglycans; molecular weight 4000–6000 |
| Mechanisms | Activates antithrombin III*; equivalent activity against factor Xa and thrombin; releases TFPI from endothelium; unable to inactivate clot-bound thrombin or FDP; inactivates fluid phase thrombin | Less activation of antithrombin III; greater activity against factor Xa than thrombin; releases TFPI for endothelium; unable to inactivate clot-bound thrombin or FDP; weaker inactivation of fluid-phase thrombin |
| Pharmacokinetics | Variable binding to plasma proteins, endothelial cells, and macrophages leads to unpredictable anticoagulant effects (less available to interact with antithrombin III); short half-life | Minimal binding to plasma proteins, endothelial cells, and macrophages leads to predictable anticoagulation; longer half-life |
| Laboratory monitoring | Unpredictable anticoagulant effects; use aPTT or ACT | Unable to use aPTT or ACT except in renal failure to body weight <50 kg or >80 kg; use anti-factor-Xa levels |
| Clinical uses | Venous thrombosis; unstable angina, acute myocardial infarction, ischemic stroke, PCI | Venous thrombosis in surgery and trauma patients, unstable angina, ischemic stroke. No advantage during PCI |
| Reversal | Protamine neutralizes antithrombin activity |



