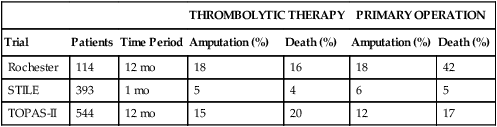
Three multicenter randomized trials were published in the 1990s comparing thrombolysis with open surgery for arterial occlusion (Table 1). TABLE 1
Anticoagulant and Lytic Therapy for Arterial Thromboembolism in Extremities
Thrombolysis and Results
Outcome Studies of Thrombolysis versus Primary Operation
THROMBOLYTIC THERAPY
PRIMARY OPERATION
Trial
Patients
Time Period
Amputation (%)
Death (%)
Amputation (%)
Death (%)
Rochester
114
12 mo
18
16
18
42
STILE
393
1 mo
5
4
6
5
TOPAS-II
544
12 mo
15
20
12
17
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Thoracic Key
Fastest Thoracic Insight Engine
