The development of atrial fibrillation (AF) after cardiac surgery is a major complication, occurring in 10% to 65% of patients. Despite the increasing number of studies on this issue, the pathophysiologic mechanisms leading to the postoperative AF after cardiac surgeries have not been precisely elucidated; however, some pathogenesis, including the electrophysiological remodeling of atrium, inflammation, and oxidative stress, have been hypothesized to be involved in this process. It has been postulated that inflammation has a paramount role in the perpetuation of AF after cardiac surgery. Moreover, using cardiopulmonary bypass at cardiac surgery leads to complement activation and the subsequent elevation of CRP.
I read the report by Elgendy et al about the effect of statins on decreasing AF after coronary artery bypass grafting (CABG). They showed that statin pretreatment reduces the development of AF after CABG (odds ratio 0.42, 95% CI 0.27 to 0.66, p <0.0001). Their meta-analysis revealed that this effect was only significant in those who received atorvastatin but not rosuvastatin. Although their findings are of great importance in clinical practice, they have not added any information regarding the probable mechanisms through which statins may prevent AF developing after CABG. In this regard, I have done a review of the studies used in their meta-analysis to explore the anti-inflammatory role of statins in the prevention of AF after cardiac surgery.
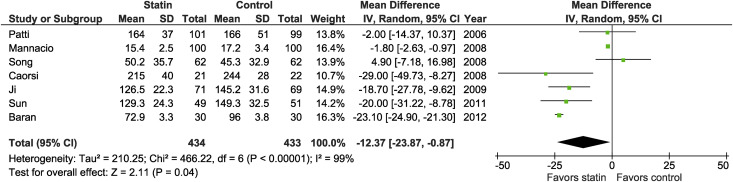
Seven of 12 studies reported the postoperative level of C-reactive protein (CRP). Pooled results demonstrated that statins decreased the postoperative CRP levels compared with control groups (mean difference in mg/L, relative risk [RR] −12.37, 95% CI −23.87 to −0.87, p = 0.04, I 2 = 99%; Figure 1 ). In addition, atorvastatin was associated with greater decrease in the CRP levels compared to other statins (RR −21.91, 95% CI −23.62 to −20.20, p <0.00001 vs RR −5.64, 95% CI −6.38 to −4.90, p <0.00001) and showed less heterogeneity as well (I 2 = 87% vs I 2 = 99%). Even after excluding studies without predefined AF monitoring methods or not placebo-controlled trials, heterogeneity related to the CRP remained substantial. This heterogeneity may be caused by clinical heterogeneity, because so many factors may be interfered with the CRP levels, and time to reach the CRP peak values differed among studies from 6 hours to 3 days.