Anterior Compartment Mass
Robert B. Carr, MD
DIFFERENTIAL DIAGNOSIS
Common
Lymphoma
Germ Cell Tumor
Teratoma
Seminoma
Thyroid Mass
Thymoma
Thymic Hyperplasia
Lipomatosis
Metastasis
Less Common
Thymic Mass
Thymic Carcinoma
Thymic Carcinoid
Thymic Cyst
Parathyroid Mass
Rare but Important
Thymolipoma
Lymphangioma
Nonseminomatous Germ Cell Tumor
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Anatomy of anterior compartment
Radiologic description is based upon radiographic landmarks as defined by Fraser and Pare; note this differs from surgical description
Anterior border is sternum, and posterior border is anterior margin of vertebral column
Normal contents: Thymus, ascending aorta, great vessels, part of main pulmonary artery, heart, pericardium, lymph nodes, adipose tissue
CT is invaluable for determining site of origin and tissue characterization
Helpful Clues for Common Diagnoses
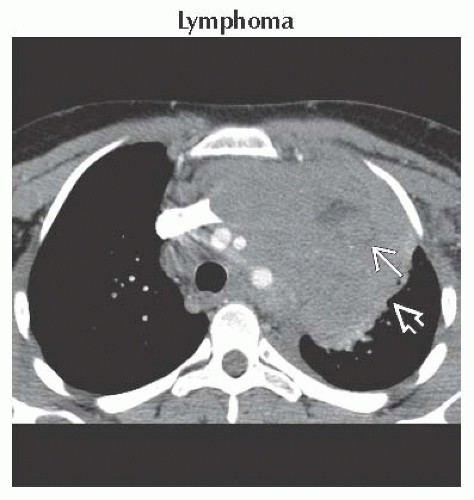
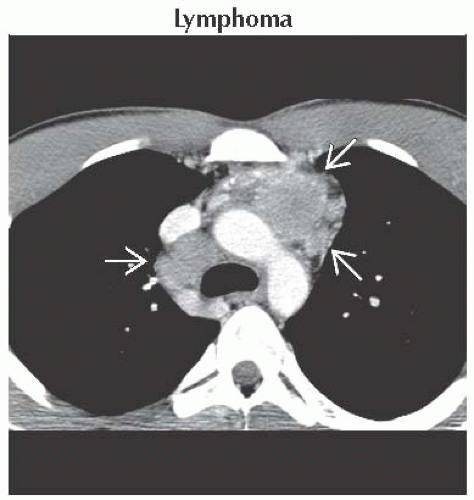
Lymphoma
Hodgkin disease (HD) more common than non-Hodgkin lymphoma (NHL) within anterior compartment
Enlarged lymph nodes or nodal mass, usually displaying homogeneous soft tissue attenuation
Necrosis is occasionally present, usually detected after contrast administration
HD commonly involves several contiguous nodal groups in thorax
Involvement of single nodal group is more common with NHL
Germ Cell Tumor
Most common age is 2nd-4th decades
More than 80% are benign
Teratoma
Most common benign germ cell tumor, though can be malignant
Display cystic areas, soft tissue, fat, and calcification
Fat-fluid level is diagnostic but usually not present
Seminoma
Most common malignant germ cell tumor and usually in males
Large homogeneous mass, which can have small focal areas of decreased attenuation
Thyroid Mass
Caused by inferior extension of thyroid lesion
Direct connection to thyroid is usually evident on CT
High attenuation on noncontrast CT is due to iodine content
Differentiation of goiter and tumor may not be possible
Thymoma
Most common in 6th decade
Associated with myasthenia gravis
Round or lobulated and usually homogeneous
Possible areas of necrosis, hemorrhage, calcification, and cyst formation
Does not conform to normal thymic contour and may be unilateral
Classified as invasive or noninvasive based upon invasion of adjacent structures (including vessels, heart, and pericardium); determination not always possible with CT
Pleural spread often produces multiple pleural implants
Thymic Hyperplasia
Associated with recovery from chemotherapy or burn (thymic rebound) in children and young adults
Associated with Grave disease, myasthenia gravis, red cell aplasia, and other conditions in adults
Thymic rebound often visible on chest radiograph; correlate with clinical history
Enlarged thymus with normal homogeneous attenuation on CT
Lipomatosis
Excessive unencapsulated fat in mediastinum associated with Cushing syndrome, steroids, obesity
Smooth, symmetric mediastinal widening on chest radiograph
Homogeneous increased amount of mediastinal fat with smooth margins on CT
Metastasis
Lung and breast primaries are common
May involve thymus or mediastinal lymph nodes
Appearance is nonspecific
Helpful Clues for Less Common Diagnoses
Thymic Carcinoma
Large mass that can have areas of necrosis
Similar to thymoma in appearance, but distant metastases are far more common than with thymoma
Metastases often involve lungs, skeleton, liver, and brain
Thymic Carcinoid
Commonly secretes ACTH, which results in Cushing syndrome
Appears similar to thymoma on imaging, though typically more aggressive
Thymic Cyst
Care should be taken not to confuse with cystic neoplasm
Nonenhancing, thin-walled, water density, no soft tissue component
Parathyroid Mass
Normal glands are not visible on CT
Ectopic glands often found in thymic bed
Cannot distinguish adenoma, hyperplasia, and carcinoma on CT
Helpful Clues for Rare Diagnoses
Thymolipoma
Most common age is 1st-4th decades
Usually asymptomatic and large at time of detection
May appear to drape over heart on chest radiograph
Primarily fat density on CT with strands of soft tissue attenuation
Lymphangioma
Usually congenital and often presents in childhood
Well circumscribed with homogeneous water attenuation
May wrap around mediastinal structures, such as great vessels
Nonseminomatous Germ Cell Tumor
Aggressive neoplasms with poor prognoses
Infiltrative and heterogeneous with areas of hemorrhage and necrosis
Image Gallery
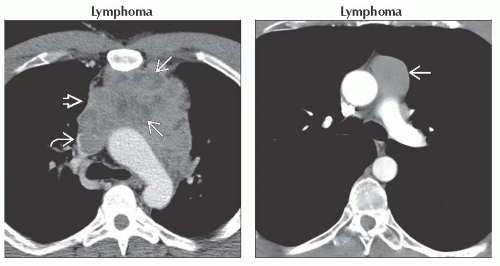 (Left) Axial CECT shows a large nodular mass in the anterior mediastinum
 with numerous areas of internal necrosis with numerous areas of internal necrosis  . Note invasion of the superior vena cava . Note invasion of the superior vena cava  . Biopsy revealed non-Hodgkin lymphoma. (Right) Axial CECT shows a homogeneous anterior mediastinal mass in the prevascular space . Biopsy revealed non-Hodgkin lymphoma. (Right) Axial CECT shows a homogeneous anterior mediastinal mass in the prevascular space  . This lesion was radiographically occult and is biopsy-proven non-Hodgkin lymphoma. . This lesion was radiographically occult and is biopsy-proven non-Hodgkin lymphoma.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|