INDICATIONS/CONTRAINDICATIONS
Nonsmall cell lung cancers invading the thoracic inlet account for fewer than 5% of all bronchial carcinomas. These tumors arise from upper lobe and tend to invade the parietal pleura, endothoracic fascia, subclavian vessels, brachial plexus, vertebral bodies, and first ribs. Their clinical features depend on their location: tumors located anterior to the anterior scalene muscle most likely invade superficial muscles, veins, and the anterior part of the first rib; tumors located between the anterior and middle scalene muscles most likely invade scalene muscles, the phrenic nerve, the subclavian artery, and the brachial plexus; lastly, tumors lying posterior to the middle scalene muscle may invade T1nerve root, the posterior aspect of the subclavian and vertebral arteries, paravertebral sympathetic chain, and the spine. Because of the peripheral location of these lesions, pulmonary symptoms, such as cough, hemoptysis, and dyspnea, are uncommon in the initial stages of the disease. Although it was believed for many years that these tumors were not amenable to surgery, it has been provided evidence that en bloc resection of the chest wall and the involved adjacent structures as well as lobectomy and mediastinal lymph nodes dissection could achieve long-term survival and should be considered as the standard of care in selected patients in as part of a multimodality approach.
The most important factor for long-term survival is the complete R0 resection of the tumor. Hence, care must be paid during the preoperative workup to rule out patients for whom complete resection seems impossible based on chest and cervical CT scan and magnetic resonance imaging (MRI). Other contraindications to resection include extrathoracic metastasis, invasion of the brachial plexus above the C8nerve root, invasion of the vertebral canal and the sheath of the medulla, massive invasion of the scalene muscles and extrathoracic muscles, mediastinal (N2) lymph nodes metastasis, and significant cardiopulmonary disease.
Because the posterior approach does not allow direct and safe control for complete oncologic clearance of all anatomic structures that compose the thoracic inlet (i.e., phrenic nerve, subclavian vessels, vertebral artery, brachial plexus), superior sulcus lesions extending to the thoracic inlet should be resected by the anterior transcervical approach. Of interest, upper lobectomy, mediastinal lymph nodes dissection, and anterolateral aspects of the upper thoracic vertebrae exposure are possible through this approach avoiding the need of any additional approach to perform the resection if the spine is not involved.
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
Any patient presenting with suspected involvement of the thoracic inlet by a lung tumor should undergo a careful and detailed preoperative evaluation to establish the diagnosis of bronchial carcinoma and assess operability. First, the diagnosis is rarely established by bronchoscopy but more often by transthoracic fine-needle aspiration. Cervical and chest CT scan, brain imaging, upper abdomen CT scan (adrenal glands), and 18F-Fluorodeoxyglucose positron emission tomography (FDG PET) scan are performed for staging purpose. If evidence of ipsilateral mediastinal lymph node involvement is found on CT scan or PET scan (clinical N2 disease), mediastinoscopy or EndoBronchial UtraSound (EBUS) will be required to prove pathologic N2 disease.
Neurologic examination and MRI delineate the tumor’s extension to the brachial plexus, phrenic nerve, and epidural space. Cervical arteries and venous duplex scan screens for any cerebrovascular disorders that may contraindicate sacrifice of the vertebral artery, but also evaluates any vascular tumoral invasion since there are usually no specific symptoms of vascular invasion in these patients. In case of suspected vascular invasion based on duplex scan and CT scan, subclavian vessels angiogram is needed to complete the preoperative workup.
The initial evaluation also includes all preoperative cardiopulmonary functional tests routinely performed before any major lung resection: Pulmonary function tests, ventilation/perfusion scan, echocardiography, and flexible bronchoscopy.
 SURGERY
SURGERY
Double-lumen tube insertion is required for intraoperative one lung ventilation. Its positioning is controlled by flexible bronchoscopy. An arterial line is inserted opposite to the tumor side and at least two peripheral venous lines may be used for volume expansion as necessary. Urine catheter serves as monitoring the patient loading during this long procedure.
Positioning
The patient is placed in a supine position, both arms along the body, with the neck hyperextended and the head turned away from the involved side. A bolster behind the shoulder helps in elevating the operative field. The skin from the mastoid downward to the ombilic and from the midaxillary line laterally to the contralateral midclavicular line medially is prepped with a chlorhexidine–alcohol or povidone–iodine solution and then draped with sterile sheets. The operating surgeon stands on the tumor side while the assistant is on the contralateral side. Care must be paid to manage space above the shoulder and the head of the patient allowing the operating surgeon to look down to the chest through the cervical incision. Finally, a bar is placed at the level of the hip to hold the chest retractor.
Technique
The anterior approach is a cervicothoracic incision including a vertical presternocleidomastoid incision carried horizontally below the clavicle up to the deltopectoral groove (Fig. 29.1). To increase the exposure, the interception between the vertical and horizontal branches of the L-shaped incision is lowered to the level of the second or third intercostal space, depending on tumor extent.
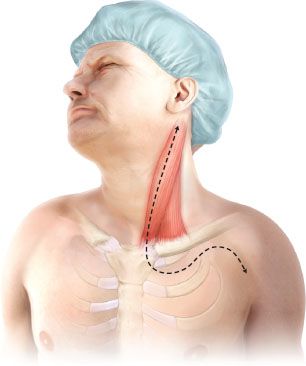
Figure 29.1 The anterior approach skin incision is a cervicothoracic incision including a vertical presternocleidomastoid incision carried horizontally below the clavicle up to the deltopectoral groove. Depending of the tumor extent, the horizontal part of the incision could be lowered to the third rib.
The operation starts with the presternocleidomastoid incision. The jugular veins are dissected first. Division of the distal part of external and anterior jugular veins facilitates visualization of the venous confluence at the origin of the innominate vein. Once the inferior belly of the omohyoid muscle is divided, the scalene fat pad is dissected and pathologically examined to rule out scalene lymph node metastasis. On the left side, ligation of the thoracic duct is usually required. Inspection of the ipsilateral superior mediastinum after division of the sternothyroid and sternohyoid muscles is then made by the operator’s finger along the tracheoesophageal groove. The tumor’s extension to the thoracic inlet is then carefully assessed. We recommend continuing with horizontal incision and then resection of the medial half of the clavicle only if the tumor is deemed resectable.
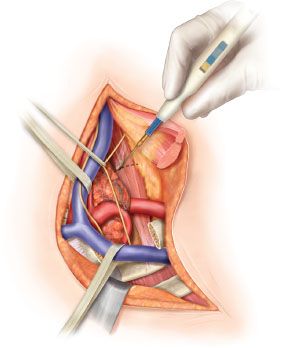
The sternal attachment of the sternocleidomastoid muscle is divided. The cleidomastoid muscle along with the upper digitations of the pectoralis major muscle are scraped from the clavicle. A myocutaneous flap is then folded back and the internal fourth of the clavicle is resected, providing full exposure of the neck and cervicothoracic junction (Fig. 29.2). At this stage, the pleural space is opened at the level of the second or third intercostal space to rule out any tumor spreading.
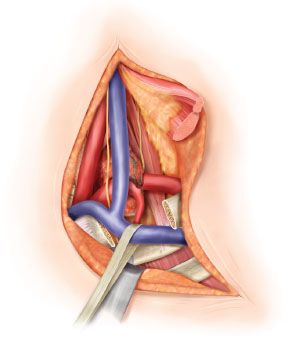
Figure 29.2 The sternal attachment of the sternocleidomastoid muscle is divided. The cleidomastoid muscle along with the upper digitations of the pectoralis major muscle are scraped from the clavicle. A myocutaneous flap is then folded back and the internal fourth of the clavicle is resected, providing full exposure of the neck and cervicothoracic junction. The internal jugular and the subclavian veins are dissected first. Once the inferior belly of the omohyoid muscle is divided, the scalene fat pad is dissected and retracted laterally given the anterior scalenus and the phrenic nerve exposure. On the left side, ligation of the thoracic duct is usually required.