Stent thrombosis is a catastrophic occurrence burdened by a high mortality rate and a tendency to recur. We sought to evaluate the angiographic risk factors for recurrent stent thrombosis (rST) in a subpopulation of 91 Outcome of PCI for stent-ThrombosIs Multicenter STudy (OPTIMIST) patients who underwent quantitative angiographic evaluation by an independent core laboratory. The Academic Research Consortium criteria were used for rST adjudication. A multivariate Cox proportional hazards model was applied to estimate the hazard ratios and the corresponding 95% confidence intervals for the occurrence of Academic Research Consortium-defined, definite rST (primary end point), definite or probable rST (secondary end point), and definite or probable or possible rST (secondary end point). A total of 8 definite rST events occurred during a median follow-up of 244 days (range 165 to 396), of which 5 were early and 3 were late. In the multivariate model, a residual thrombus score of ≥3 (hazard ratio 6.5, 95% confidence interval 1.4 to 30.7, p = 0.017) and a larger postprocedural reference vessel diameter (hazard ratio 4.5, 95% confidence interval 1.5 to 13.3, p = 0.006) were significantly associated with the primary end point. When the same model was applied to the 15 definite and probable rST events, only a residual thrombus score of ≥3 (hazard ratio 7.8, 95% confidence interval 2.5 to 24.5, p <0.001) was significantly associated with rST. Finally, when possible rST events were included (18 patients), a residual thrombus score of ≥3 remained associated with the dependent variable (hazard ratio 6.1, 95% confidence interval 2.0 to 18.2, p = 0.001), along with a larger postprocedural reference vessel diameter. In conclusion, when performing percutaneous coronary intervention for stent thrombosis, the residual thrombus burden and larger reference vessel were potent risk factors for rST.
Despite the recent improvements in percutaneous coronary intervention technique, materials and adjunctive pharmacology, stent thrombosis (ST) remains a major limitation of this technique. Large, multicenter registries have clarified that a ST incidence of about 1% to 2% during the first year is to be expected, followed by 0.5% annually and perhaps greater for drug-eluting stents compared to bare metal stents in the case of very late ST. Although few reports have focused on the procedural variables related to the outcome of patients with angiographically established ST, no previous study has used core laboratory-based quantitative coronary angiographic analysis to establish which angiographic variables are associated with recurrent ST (rST), an event with a frequency as great as 20% at 3 years and peaking during the first 30 days. In a planned subanalysis, we used the Outcome of PCI for stent-ThrombosIs Multicenter STudy (OPTIMIST) database to identify the angiographic predictors of rST.
Methods
The OPTIMIST was a nonsponsored registry enrolling consecutive patients with ST treated by percutaneous coronary intervention (PCI) from 11 centers. The study protocol and the main analysis have been previously published. The detailed inclusion and exclusion criteria for the main study have been previously published. Centralized blind-to-outcome angiographic analysis, in particular, was performed at the Rome Heart Research (Rome, Italy). Only the baseline and final post-PCI views, extrapolated by the coordinating center, were sent for analysis to warrant angiographic analyses fully independent of the knowledge of the PCI strategy and outcome. The analyzed variables included
Anterograde coronary flow according to standard Thrombolysis In Myocardial Infarction (TIMI) criteria
Corrected TIMI frame count according to Gibson et al
Thrombus score according to the TIMI study group (0, no angiographic characteristics of thrombus present; 1, possible thrombus present, with angiography characteristics such as reduced contrast density, haziness, irregular lesion contour, or a smooth convex “meniscus” at the site of total occlusion suggestive, but not diagnostic, of thrombus; 2, definite thrombus, with the greatest dimensions ≤1/2 the vessel diameter; 3, definite thrombus, with greatest linear dimension >1/2 but <2 vessel diameters; 4, definite thrombus, with the largest dimension ≥2 vessel diameters; and 5 = total occlusion)
Myocardial blush grade according to van’t Hof et al
Quantitative coronary angiography analysis (CMS Medis Imaging System, Wallingford, Connecticut) of the target lesions before and after PCI
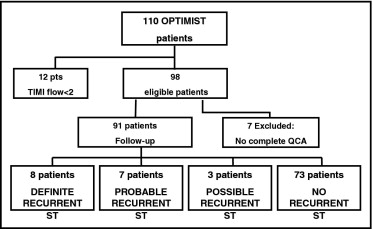
In the present subanalysis, which focused on the angiographic predictors of recurring stent thrombosis, we had to exclude those patients who had not undergone a complete angiographic workup. Of the original 110 patients, 19 patients were not included because of unsuccessful reperfusion (TIMI flow 0 or 1 at the end of the index procedure) in 10 patients, incomplete angiographic analysis in 7 patients, and both conditions in 2 patients. Figure 1 depicts the study flow of the patients.
The following Academic Research Consortium definitions of ST according to the interval between PCI and thrombosis of the stent were used: early (0 to 30 days), late (>30 days to 1 year), and very late (>1 year). Myocardial infarction (MI) included both Q-wave and non–Q-wave MI and was defined as ischemic symptoms and/or ischemic electrocardiographic changes plus elevation of creatine-kinase MB or troponin T or I levels to greater than the normal laboratory values. The following Academic Research Consortium definitions of rST during follow-up were used: definite (angiographically or autopsy-confirmed ST), probable (any unexplained death within the first 30 days or any myocardial infarction in the territory of the stent and in the absence of any other obvious cause), and possible (any unexplained death >30 days after PCI).
The predefined primary end point was the incidence of recurrent “definite” ST according to the Academic Research Consortium criteria. The secondary end points included the cumulative rate of definite and probable rST and of definite, probable, and possible rST. The clinical and procedural characteristics, angiographic results, and clinical follow-up data are presented for the subgroups of patients with rST and non-rST. Continuous variables are presented as the median and interquartile ranges and were compared using Student’s t test or the Wilcoxon-Mann-Whitney test, as appropriate. Categorical variables are summarized as counts and percentages and were compared using the chi-square test or Fisher’s exact test, as appropriate. The incidence of events over time was studied using the Kaplan-Meier method and compared using log-rank tests. The predictors of rST were assessed using a stepwise multivariate Cox proportional hazards model to estimate the hazard ratios and corresponding 95% confidence intervals). First, a univariate analysis was performed. Next, the variables with a probability value <0.10 plus the variables that were predictive of 6-month mortality in the OPTIMIST main analysis (ie, very late thrombosis, the absence of optimal reperfusion, and additional stent implantation) were included, adopting a forward stepwise selection. Nonfatal events that were not a part of an end point were not a reason for censoring. All authors had full access to, and take full responsibility for, the integrity of the data, and all authors have read and agreed to the manuscript as written. A 2-tailed, p value <0.05 was established as the level of statistical significance for all tests. Analyses were performed using Statistical Package for Social Sciences for Windows, version 15.0 (SPSS, Chicago, Illinois).
Results
Detailed characteristics of the whole OPTIMIST population have been previously published. The clinical and angiographic (at the first ST) characteristics of the studied sample (91 patients) are listed in Tables 1 and 2 . As per the inclusion criteria, only those patients with postprocedural TIMI 2 or 3 flow were included. Figure 1 shows the flow of the study participants. The first ST treatment details, including the use of glycoprotein IIb/IIIa inhibitors, percentage of new stent implantation, percentage of drug-eluting stents used, percentage of very late thromboses, and percentage of optimal reperfusion after PCI were not significantly different in our sample from the data for the whole OPTIMIST study (data not shown).
| Variable | All Patients (n = 91) | rST (n = 8) | Non-rST (n = 83) | p Value |
|---|---|---|---|---|
| Mean age ± SD (years) | 66.0 ± 11.5 | 63.0 ± 11.5 | 66.1 ± 11.6 | 0.4 |
| Men | 64 (70%) | 5 (62.5%) | 59 (71%) | 0.7 |
| Malignancy | 11 (12%) | 1 (12.5%) | 10 (12%) | 1 |
| Hypertension | 60 (66%) | 7 (87.5%) | 53 (64%) | 0.2 |
| Family history of coronary artery disease | 22 (24%) | 3 (37.5%) | 19 (23%) | 0.4 |
| Smokers | 40 (44%) | 5 (62.5%) | 35 (42%) | 0.3 |
| Hypercholesterolemia | 45 (49%) | 2 (25%) | 43 (52%) | 0.2 |
| Diabetes | 26 (29%) | 3 (37.5%) | 23 (28%) | 0.5 |
| Indication for percutaneous coronary intervention | 0.7 | |||
| Elective | 44 (48%) | 3 (37.5%) | 41 (49%) | |
| Acute coronary syndrome | 47 (52%) | 5 (62.5%) | 42 (51%) | |
| Very late thrombosis | 6 (7%) | 0 (0%) | 6 (7%) | 0.8 |
| Glycoprotein IIb/IIIa inhibitor use | 66 (73%) | 8 (100%) | 58 (70%) | 0.2 |
| Hemodynamic instability | 16 (18%) | 0 (0%) | 16 (19%) | 0.3 |
| Intra-aortic balloon pump | 10 (11%) | 0 (0%) | 10 (12%) | 0.3 |
| Thrombosed stent | ||||
| Bare metal stent | 48 (53%) | 4 (50%) | 44 (53%) | 0.7 |
| Drug-eluting stent | 43 (47%) | 4 (50%) | 39 (47%) | 0.6 |
| Variable | All Patients (n = 91) | rST (n = 8) | Non-rST (n = 83) | p Value |
|---|---|---|---|---|
| Occluded vessel before percutaneous coronary intervention | 74 (81%) | 8 (100%) | 66 (79%) | 0.34 |
| Quantitative coronary angiography | ||||
| Minimum lumen diameter (mm) | ||||
| Before percutaneous coronary intervention | 0.1 ± 0.3 | 0.0 ± 0.0 | 0.1 ± 0.3 | 0.15 |
| After percutaneous coronary intervention | 2.6 ± 0.6 | 3.2 ± 0.6 | 2.5 ± 0.6 | 0.03 |
| Reference vessel diameter (mm) | ||||
| Before percutaneous coronary intervention | 2.6 ± 0.6 | 2.7 ± 0.7 | 2.6 ± 0.7 | 0.50 |
| After percutaneous coronary intervention | 2.9 ± 0.6 | 3.5 ± 0.5 | 2.9 ± 0.5 | 0.01 |
| Residual stenosis after percutaneous coronary intervention (%) | 12.2 ± 11.5 | 7.8 ± 6.2 | 12.7 ± 12.0 | 0.26 |
| Thrombolysis In Myocardial Infarction 3 flow after percutaneous coronary intervention | 75 (82%) | 7 (87%) | 68 (82%) | 0.7 |
| Myocardial blush grade 2–3 after percutaneous coronary intervention | 61 (67%) | 7 (87%) | 54 (74%) | 0.7 |
| Thrombolysis In Myocardial Infarction 3 plus myocardial blush grade 2–3 after percutaneous coronary intervention | 61 (67%) | 7 (87%) | 54 (74%) | 0.7 |
| Corrected Thrombolysis In Myocardial Infarction frame count | ||||
| Before percutaneous coronary intervention | 90 ± 27 | 100 ± 0 | 88.5 ± 28.5 | 0.25 |
| After percutaneous coronary intervention | 18.9 ± 15.3 | 27.5 ± 21.0 | 18.0 ± 14.0 | 0.4 |
| Thrombus score | ||||
| Before percutaneous coronary intervention | 4.7 ± 0.7 | 5.0 ± 0.0 | 4.7 ± 0.7 | 0.18 |
| After percutaneous coronary intervention | 0.6 ± 1.1 | 1.4 ± 1.5 | 0.6 ± 1.0 | 0.05 |
| Thrombus score ≥3 after percutaneous coronary intervention | 9 (11%) | 3 (37.5%) | 6 (7%) | 0.03 |
| Any residual thrombus | 32 (35%) | 5 (62.5%) | 27 (33%) | 0.1 |
| Bifurcation | 19 (21%) | 1 (12.5%) | 18 (22%) | 0.8 |
| Stent hypoexpansion | 22 (24%) | 0 (0%) | 22 (26.5%) | 0.2 |
| Severe calcium | 8 (9%) | 0 (0%) | 8 (10%) | 0.4 |
| Stent in left anterior descending artery | 51 (56%) | 4 (50%) | 47 (56%) | 0.7 |
| Total stent length (mm) | 23 (18–30.5) | 28 (20.5–44) | 23 (16–30) | 0.069 |
| Stent diameter (mm) | 3.0 (2.5–3.0) | 3.25 (2.8–3.5) | 3.0 (2.5–3.0) | 0.055 |
| Maximum balloon diameter (mm) | 3.0 (2.5–3.3) | 3.0 (2.5–4.0) | 3.0 (2.5–3.0) | 0.5 |
| Maximum dilating pressure (atm) | 14 (12–16) | 14 (11.5–14) | 16 (14–18) | 0.18 |
| Residual dissection | 5 (5%) | 0 (0%) | 5 (6%) | 0.5 |
| Adjunctive device used | 24 (28%) | 4 (50%) | 20 (24%) | 0.2 |
| Additional stent implantation | 43 (47%) | 5 (63%) | 38 (46%) | 0.4 |
| Drug-eluting stent use | 19 (21%) | 1 (20%) | 18 (47%) | 0.3 |
Follow-up data were obtained for all 91 patients at 30 days and >6 months. Of the 91 patients presenting with a first ST, 15 (16%) had died during the follow-up period. The median occurrence of death was 15 days (interquartile range 5 to 144). Moreover, 14 patients (15%) presented with a recurrent MI and 18 (20%) underwent repeat PCI. The median interval was 19 days (interquartile range 6 to 126) to recurrent MI and 6 days (interquartile range 1 to 126) for repeat PCI. Recurrent MI developed in 7 patients (50%) because of rST. During a median follow-up of 244 days (interquartile range 165 to 396), 8 definite rST events occurred, of which 5 were early (3 leading to cardiac death preceded by cardiogenic shock, and 2 resolved with repeat PCI) and 3 were late (of which, only 1 was treated with repeat PCI). The median interval to definite rST was 8 days (interquartile range 6 to 138). Additionally, 7 probable rST events occurred, of which 4 were early and 3 were late. The median interval to definite or probable rST was 8 days (interquartile range 6 to 138). Finally, 3 possible rST events occurred, all late events. No iterative rST occurred during the follow-up period. The cumulative incidence of the primary and the 2 secondary end points is shown in Figure 2 .
Table 3 depicts the 3 multivariate Cox proportional hazard models for the 3 end points. When the primary end point of definite rST was evaluated, a residual thrombus score of ≥3 was significantly associated with the primary outcome measure, as was a larger postprocedural reference vessel diameter. When the same model was applied to the 15 definite and probable rSTs, again, a residual thrombus score of ≥3 was significantly associated with rST. Finally, when even possible rST was considered (18 patients), a residual thrombus score of ≥3 remained associated with the dependent variable, as did a larger reference vessel diameter. Figure 2 depicts the long-term cumulative incidence of the primary and secondary end points according to the presence of a residual thrombus score of ≥3. Finally, to check for consistency, the definition of “residual thrombus” was enlarged to include “any residual thrombus” (eg, including patients with low-to-moderate thrombus [grade 1 to 2]). Overall, 32 patients (35%) presented with any grade of residual thrombus, with a trend toward an increased incidence in patients who subsequently developed definite rST (62.5% vs 33%, p = 0.1). When this variable was substituted for a residual thrombus score of ≥3 in the first step of the multivariate model, it was selected in the second step of the forward selection and became significant in the multivariate model, significantly predicting definite rST (hazard ratio 13.1, 95% confidence interval 1.4 to 120.0, p = 0.003), definite and probable rST (hazard ratio 3.9, 95% confidence interval 1.2 to 13.9, p = 0.026), and definite, probable, and possible rST (hazard ratio 5.3, 95% confidence interval 1.6 to 17.7, p = 0.006).



