Shortening symptom-to-reperfusion time improves prognosis in patients with ST-segment elevation myocardial infarction. Accordingly, current guidelines target a door-to-balloon time <90 minutes, irrespective of symptom-to-door time; nevertheless, the relation between door-to-balloon and symptom-to-door time and its potential impact on myocardial salvage remains largely unknown. We investigated the influence of door-to-balloon guideline fulfillment on myocardial salvage in patients presenting with different symptom-to-door times. Contrast-enhanced magnetic resonance study was performed acutely to measure infarct size in 172 patients admitted for primary percutaneous coronary intervention of their first ST-segment elevation myocardial infarction to 2 tertiary hospitals. The Bari score was adapted to quantify the angiographic area at risk, and the myocardial salvage index (MSI) was computed as percent area at risk that spared necrosis. Increased symptom-to-balloon time was associated with a significant decrease in MSI only within the first 5 hours (p <0.001). Accomplishment of a target door-to-balloon <90 minutes was associated with a significant increase in MSI only in patients presenting within the first hour of symptom onset (48.5 ± 30.9 vs 29.6 ± 22.3%, p <0.05). Achieving a door-to-balloon time <60 minutes further increased MSI in patients presenting within the second hour of symptoms (43.5 ± 8.6 vs 26.3 ± 20.5%, p <0.01). In conclusion, myocardial salvage progressively decreases up to 5 hours after symptom onset. However, the benefit of the recommended door-to-balloon time appears to be confined to patients presenting within 1 hour of symptom onset.
Timely reperfusion of the infarct-related coronary artery through percutaneous coronary intervention (PCI) or fibrinolysis decreases myocardial damage, increases left ventricular (LV) function recovery, and decreases morbidity and mortality in patients with ST-segment elevation myocardial infarction (STEMI). Delays in PCI delivery since presentation to the hospital, known as door-to-balloon time, have also been associated with poorer outcomes in many but not all studies. In the National Registry of Myocardial Infarction 3 and 4, this relation was shown to be consistent and independent of time from symptom onset to presentation at the hospital, termed the “symptom-to-door time,” whereas other smaller studies have suggested that such association only exists in patients presenting soon (<2 hours) after onset of symptoms. Nevertheless, current guidelines target a delay <90 minutes from first medical contact to balloon inflation and a door-to-balloon time <90 minutes for self-transported patients admitted to the emergency department, irrespective of symptom-to-door time. We conducted an observational angiographic and cardiac magnetic resonance study to determine the influence of in-hospital delays on myocardial salvage. We hypothesized that a short door-to-balloon time (<90 minutes as recommended by current guidelines) would result in a measurable increase in myocardial salvage only in patients presenting within the first 2 hours of symptom onset.
Methods
From July 1999 to December 2006, 514 patients with STEMI were treated with PCI at Northwestern Memorial Hospital (Chicago, Illinois). Similarly, from January 2007 to July 2008, 262 patients were treated at Hospital Clinic i Provincial de Barcelona (Barcelona, Spain). We did not include subjects with unstable hemodynamics, contraindications to undergo contrast-enhanced cardiac magnetic resonance (ce-CMR) examination, and previous MI. A total of 210 patients were prospectively included in the study. All subjects had a ce-CMR study done within 10 days of admission as part of several studies assessing LV remodeling and myocardial viability after STEMI. Subjects were included in the study if they presented with typical chest pain lasting >30 minutes, had ≥0.2-mV ST-segment elevation in leads V 1 to V 3 or 0.1-mV elevation in other contiguous electrocardiographic leads, or suspicion of true posterior infarction and increased creatine phosphokinase-MB isoenzyme levels. In all, 87% of patients were treated in the first 12 hours, whereas the remaining patients were treated up to 24 hours after symptom onset due to persistence of chest pain and ST-segment elevation or development of heart failure. To avoid the effect of spontaneous coronary reperfusion on salvage as a confounding factor, 34 subjects with initial Thrombolysis In Myocardial Infarction grade 2 or 3 flow in the infarct related artery were excluded. We also excluded 3 subjects with incomplete ce-CMR data due to limitations in image quality and 1 subject with uncertain identification of the infarct-related artery. The remaining 172 subjects formed the study population. All subjects signed an informed consent form for the study, which was approved by the institutional review boards of the 2 hospitals.
The standard of care for each participating hospital in treating STEMI patients was applied. Primary PCI was the reperfusion strategy of choice for all patients and delivered by experienced, on-call interventional cardiologists. All patients received unfractionated heparin and aspirin and were transferred promptly to the catheterization laboratory. Patients admitted from community hospitals received intravenous heparin and aspirin. No facilitation regimen was given before hospital transfer. A total of 155 patients (90%) were treated with glycoprotein IIb/IIIa inhibitors, 29% initiated in the emergency department and 71% at time of PCI. Beta-adrenergic blocking agents and nitrates were used at the physicians’ discretion. At least 1 stent was deployed in 98% of patients, and 97% were treated with thienopyridines.
Symptom-to-door time was defined as the time between onset of ischemic symptoms to a patient’s arrival at the hospital. Door-to-balloon time was defined as the time from a patient’s arrival to the hospital to first balloon inflation. For transferred patients, door-to-balloon time was defined as admission at the referring hospital to balloon inflation at the treating hospital. For patients included before 2004, symptom-to-door and door-to-balloon times were collected from emergency room records, chart review, and cardiac catheterization laboratory records. Since January 2004, symptom-to-door and door-to-balloon times were collected prospectively from the anamnesis. Symptom-to-balloon time was calculated by summing the symptom-to-door and door-to-balloon times.
Two independent cardiologists reviewed all angiograms independently of the results of the ce-CMR images. The culprit lesion was easily identifiable during PCI based on angiographic findings of the lesion, clinical information, and immediate response to reperfusion in all cases except for 1. The jeopardized myocardium was evaluated using the modified Bari score as previously validated. Briefly, all terminating arteries supplying blood to the left ventricle were graded according to vessel length and caliber (0 = insignificant, 1 = small, 2 = medium, 3 = large), with septal branches being arbitrarily assigned a maximum of 3 U. All units affected by the culprit lesion were summed and divided by total units supplying the left ventricle to calculate the anatomic area at risk as percent total LV wall volume. Anterograde flow in the infarct-related artery was characterized using the Thrombolysis In Myocardial Infarction scoring system.
Subjects were imaged in a 1.5-T Siemens (Sonata or Avanto, Erlangen, Germany) or GE (Signa CV Imaging, Milwaukee, Wisconsin) scanner equipped with a cardiac-dedicated phased-array receiver coil. CMR studies were performed at a mean of 3.4 ± 2 days (range 1 to 9) after hospital admission. To assess LV function, a standard steady-state free precession sequence was prescribed on sequential short-axis slices throughout the left ventricle and in long-axis views. Ten to 15 minutes after intravenous administration of gadopentetate dimeglumine 0.2 mmol/kg (Berlex, Montville, New Jersey) or gadodiamide 0.2 mmol/kg (Omniscan, GE Healthcare, Madrid, Spain), contrast-enhanced images were acquired in identical contiguous short-axis slices every 10 mm and long-axis views using a standard T1-weighted segmented inversion-recovery gradient echocardiographic sequence. Inversion time, from 180 to 320 ms, was set to null normal myocardium. Matrix size was 256 pixels to cover a field of view of 320 to 440 mm, yielding a typical voxel size of 1.4 to 1.7 × 1.4 to 1.7 × 6 or 10 mm.
Using ImageJ software (National Institutes of Health, Bethesda, Maryland) an observer, masked to the catheterization results, cropped and interpolated all images by a factor of 3. Endocardial and epicardial borders on sequential short-axis cine images were traced at end-systole and end-diastole to compute LV end-systolic and end-diastolic volumes ands LV mass and ejection fraction. For short-axis contrast-enhanced images, areas of hyperenhancement were treated planimetrically as previously described. Areas of microvascular obstruction, defined as those areas with late hypoenhancement within a hyperenhanced region, were included in the total infarct area. Infarct areas on sequential short-axis slices were summed and divided by total LV myocardial volume to calculate infarct size as percent LV myocardial volume. Transmural extent of infarct for each of the 17 myocardial segments was visually scored as 0 (no infarction), 1 (1% to 25%), 2 (26% to 50%), 3 (51% to 75%), and 4 (76% to 100% of wall thickness). Mean score for transmural extent of infarct for every study was calculated by dividing the sum of hyperenhancement segmental scores by the number of segments with any hyperenhancement. Infarct size by ce-CMR was subtracted from the estimated angiographic area at risk to compute myocardial salvage, expressed as percent LV wall volume. To account for differences in anatomic area at risk, a myocardial salvage index (MSI) was computed as follows: MSI = (area at risk by angiography − infarct size by ce-CMR) × 100/area at risk by angiography, expressed as percent area at risk.
Quantitative variables are presented as mean ± SD or number (percentage). Symptom-to-balloon and door-to-balloon times are presented as median (25th to 75th percentiles). The population was divided according to a door-to-balloon time ≥90 or <90 minutes. Shapiro-Wilk test was used to confirm that MSI, but not transmural extent of infarct, followed a normal distribution. Therefore, the variable transmural extent of infarct was rank-transformed. Effect of symptom-to-balloon time on myocardial salvage and transmural extent of infarct was evaluated with 1-way analysis of variance with post hoc Bonferroni corrections and Kruskal-Wallis test, respectively. Unpaired Student’s t test or Mann-Whitney U test was used to perform comparisons of means between groups. Intra- and interobserver agreements for measuring MSI were assessed with Lin concordance correlation coefficient. SPSS 13 (SPSS, Inc., Chicago, Illinois) was used and a 2-tailed p value <0.05 was considered statistically significant.
Results
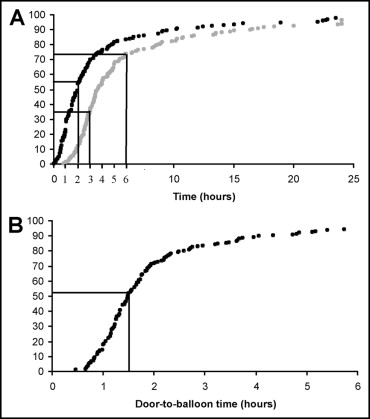
No differences in clinical characteristics were observed between the 2 participating hospitals. However, patients treated in Chicago more frequently had multivessel disease and presented with better collateral flow grades ( Table 1 ). For the entire cohort, symptom-to-door time was 120 minutes (60 to 239), door-to-balloon time was 89 minutes (69 to 132), and symptom-to-balloon time was 220 minutes (156 to 406). Most patients (93%) were admitted to the treating hospitals, whereas only 12 patients were transferred from community hospitals for primary PCI. Median door-to-balloon time was significantly longer for transferred patients (260 minutes, 218 to 388, vs 87 minutes, 68 to 126, p <0.001), leading to an overall increased symptom-to-balloon time in this group (413 minutes, 281 to 636, vs 210 minutes, 155 to 360, p <0.01). In total, 28% of patients presented to the hospital within the first hour of symptoms, and 54% presented within 2 hours. Only 34% of patients were reperfused within 3 hours of symptom onset, but up to 74% of patients were treated within 6 hours of symptom onset ( Figure 1 ). Target door-to-balloon time <90 minutes was achieved in 90 patients (52%; Figure 1 ).
| Variable | Northwestern University, Chicago (n = 100) | Hospital Clinic i Provincial de Barcelona (n = 72) | p Value |
|---|---|---|---|
| Age (years) | 58 ± 10 | 59 ± 13 | 0.3 |
| Men | 85 (85%) | 59 (82%) | 0.6 |
| Hypertension | 44 (44%) | 37 (52%) | 0.1 |
| Smoking | 50 (50%) | 45 (63%) | 0.09 |
| Dyslipidemia ⁎ | 51 (51%) | 30 (42%) | 0.2 |
| Diabetes mellitus | 16 (16%) | 14 (19%) | 0.7 |
| Multivessel coronary disease | 62 (62%) | 28 (39%) | <0.05 |
| Anterior wall infarction | 49 (49%) | 35 (49%) | 1.0 |
| Collateral grade 2 or 3 | 41 (41%) | 13 (18%) | <0.01 |
| Symptom-to-door time (minutes) | 97 (42–228) | 123 (74–240) | 0.2 |
| Door-to-balloon time (minutes) | 89 (68–133) | 90 (70–142) | 0.9 |
⁎ Treatment with statins or total cholesterol level >240 mg/dl.
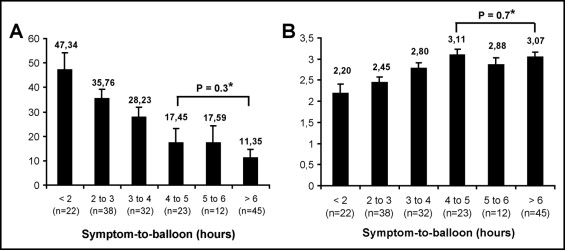
MSI progressively decreased as symptom-to-balloon time increased during the first 5 hours (p <0.001 for trend). Further increases in symptom-to-balloon time did not affect MSI ( Figure 2 ). Accordingly, increasing symptom-to-balloon time was associated with a progressive increase in mean infarct transmural extent only within the first 5 hours of symptom onset ( Figure 2 ). No major clinical differences were found between patients with door-to-balloon times ≤90 or >90 minutes ( Table 2 ). Patients with a door-to-balloon time >90 minutes tended to have larger infarcts (p = 0.1), increased infarct transmural extent (p = 0.06), and lower MSI (p = 0.1). The entire cohort was divided into 4 subgroups according to symptom-to-door time (<1, 1 to 2, 2 to 3, and >3 hours). Achieving a door-to-balloon time <90 minutes was associated with an increase in MSI (48.5 ± 30.9 vs 29.6 ± 22.3% of area at risk, p <0.01) and a significant decrease in mean infarct transmural extent (2.03 ± 0.93 vs 2.81 ± 0.77, p <0.01) only in patients presenting to the emergency room within 1 hour of symptom onset ( Figure 3 ). No significant differences were found in MSI in patients presenting after the first hour of symptoms with door-to-balloon times >90 or <90 minutes. Importantly, achievement of a door-to-balloon time <60 minutes further increased salvage in subjects presenting within the second hour of symptom onset compared to patients with a door-to-balloon time >60 minutes (43.49 ± 8.57 vs 26.35 ± 20.46%, p <0.01; Figure 4 ). Two independent observers reviewed the CMR studies and coronary angiograms in a subset of 30 randomly selected cases to test intraobserver and interobserver variabilities for measuring MSI. Intraobserver and interobserver concordance correlation coefficients were 0.94 (95% confidence interval 0.90 to 0.98) and 0.92 (95% confidence interval 0.87 to 0.97), respectively.
| Variable | Total (n = 270) | Door-to-Balloon Time (minutes) | p Value | |
|---|---|---|---|---|
| <90 (n = 90) | >90 (n = 82) | |||
| Age (years) | 58 ± 11 | 59 ± 11 | 56 ± 12 | 0.06 |
| Men | 144 (84%) | 72 (80%) | 72 (86%) | 0.3 |
| Hypertension | 81 (47%) | 47 (52%) | 34 (41%) | 0.1 |
| Smoking | 97 (56%) | 52 (58%) | 45 (54%) | 0.6 |
| Dyslipidemia | 82 (48%) | 41 (46%) | 41 (50%) | 0.7 |
| Diabetes mellitus | 30 (17%) | 15 (17%) | 15 (18%) | 0.8 |
| Multivessel disease | 91 (53%) | 48 (53%) | 43 (52%) | 0.9 |
| Anterior infarction | 85 (49%) | 41 (45%) | 44 (54%) | 0.4 |
| Collateral grade 2 or 3 | 53 (31%) | 26 (29%) | 27 (33%) | 0.6 |
| Symptom-to-door time (minutes) | 120 (60–240) | 120 (60–232) | 120 (60–267) | 0.9 |
| Symptom-to-balloon time(minutes) | 220 (156–391) | 170 (129–300) | 268 (180–473) | <0.001 |
| Area at risk (percent left ventricle) | 31.4 ± 10.5 | 31.3 ± 10.5 | 31.6 ± 10.9 | 0.9 |
| Infarct size (percent left ventricle) | 23.3 ± 11.9 | 21.9 ± 12.0 | 24.7 ± 12.1 | 0.1 |
| Myocardial salvage index (percent area at risk) | 25.5 ± 26.9 | 29.4 ± 28.4 | 22.1 ± 24.2 | 0.1 |
| Infarct transmural extent score | 2.76 ± 0.8 | 2.65 ± 0.8 | 2.87 ± 0.75 | 0.09 |
| Microvascular obstruction | 78 (45%) | 43 (48%) | 35 (43%) | 0.4 |
| Left ventricular end-diastolic volume (ml) | 156 ± 37 | 153 ± 34 | 161 ± 40 | 0.2 |
| Left ventricular end-systolic volume (ml) | 92 ± 34 | 89 ± 31 | 96 ± 37 | 0.2 |
| Ejection fraction (%) | 42.1 ± 10.7 | 43 ± 10 | 41 ± 11 | 0.3 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


