ANESTHESIA FOR THE NEONATE WITH CONGENITAL HEART DISEASE
Introduction
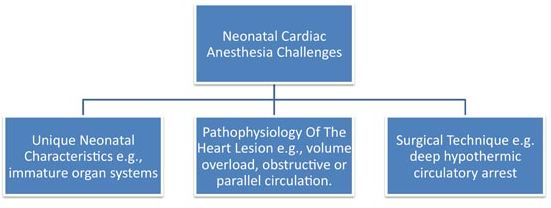
Over the last decade, enormous progress has been made with pediatric cardiac surgical techniques, cardiopulmonary bypass (CPB) strategies, anesthesia equipment, and anesthetic management making neonatal cardiac surgery much safer today. The pillars of anesthetic management for neonates with congenital heart disease (CHD) undergoing palliative or corrective surgery are understanding of unique neonatal characteristics, pathophysiology of the lesion, and estimating the impact of the associated surgical techniques (see Figure 24.1).
Figure 24.1. Neonatal cardiac anesthesia care challenges.
Unique Neonatal Characteristics
Respiratory System
A full-term neonate consumes 4 to 6 mL/kg/min of oxygen and has an immature, developing pulmonary system working at maximum capacity to support this need. At birth, neonatal lungs have only one-tenth of the alveoli compared with adult lungs. In the spontaneously breathing neonate, the cartilaginous neonatal chest wall is very compliant and does not recoil outward at end expiration with reduced ability to maintain negative intrapleural pressures. Neonatal diaphragm and intercostal muscles also have a lower percentage of the slow-twitch, highly oxidative type-1 muscle fibers and predispose the neonate to early fatigue when there is atelectasis or poor chest wall compliance.1 The very small airways are prone to obstruction with minimal secretions, causing atelectasis. Application of positive end expiratory pressure enables the neonate to maintain the lungs close to the functional residual capacity reducing the amount of atelectasis and improves oxygenation.
Cardiovascular System
At birth, the neonatal myocardium lacks sufficient contractile elements, has an immature sarcoplasmic reticulum, requires higher concentrations of extracellular calcium to achieve maximal contractility, has an underdeveloped sympathetic autonomic system, has poor compliance, and abnormal load handling characteristics. The poorly compliant heart has limited capacity to increase its stroke volume and is dependent on heart rate when faced with an increased preload. Despite these shortcomings, the qualitative relationship of the blood pressure being directly proportional to cardiac output and systemic vascular resistance (SVR) is maintained.
Nervous System
The neonatal period constitutes a period of rapid synaptogenesis in the sensorimotor complex, continuing myelination with synaptic signaling and an abundance of rapid eye movement sleep.2 This normal development is hampered in neonates undergoing cardiac surgery and 30% to 50% of the neonates experience significant neurodevelopmental (ND) delays when tested during infancy.
Renal and Hepatic Systems
At birth, kidneys have a low glomerular filtration rate regulated by a delicate balance of intrarenal vasoconstrictor and vasodilatory forces. Neonates are prone to hyponatremia (obligatory salt wasters) with the renin angiotensin system as the primary compensatory mechanism. They also suffer from a high insensible water loss that can result in hypernatremia. Complete maturation of renal function takes 6 months to 2 years.3 Neonates undergoing procedures in the cardiac catheterization suite are at increased risk of fluid overload and electrolyte imbalance due to flush fluid used for catheter exchange and de-airing. Fluid management should be guided by frequent assessment of electrolytes.
Hepatic biotransformation is immature at birth. Coagulation factors produced by the liver are at lower concentrations. Neonates have low glycogen stores, increasing the risk of hypoglycemia.
Temperature Control
Physiological characteristics of neonates, such as lack of subcutaneous fat and increased surface area to body mass ratio, make heat loss comparatively easy and increases the risk of hypothermia.4 In addition, ability to control temperature is immature in the neonates further increasing the risk of temperature imbalance.
Vascular Access Challenges
Vascular access is at a premium in neonates and is challenging due to very small size of vessels. An ability to place or replace umbilical vascular access should be sought by the anesthesiologist taking care of a neonate. Recent introduction of ultrasound use for both peripheral and central vascular access has demonstrated increased safety and rate of successful cannulation in trained hands.
Pathophysiology of Heart Lesions
To discern the magnitude of intracardiac shunts, it is important for the anesthesiologist to understand the physiology of total and effective blood flow. Effective blood flow is the quantity of venous blood flow from one circulatory system to reach the arterial system of the other circulatory system. Effective pulmonary and effective systemic blood flows are always equal regardless of the complexity of the lesion. Total pulmonary blood flow (Qp) is the sum of effective pulmonary blood flow and recirculated pulmonary blood flow. Total systemic blood flow (Qs) is the sum of effective systemic blood flow and recirculated systemic blood flow. The total blood flows do not have to be equal and the ratios (Qp:Qs) determine the magnitude of shunting.
Shunting with Volume Overload and No Obstruction
Isolated left-to-right shunts result in volume overload of the heart and are typically acyanotic. Usually right heart volume overload and dilatation is seen if the shunt is proximal to the mitral valve, for example, atrial septal defect (ASD), partial or total anomalous pulmonary venous return (TAPVR). On the other hand, left heart volume overload occurs if the shunt is distal to the mitral valve, for example, ventricular septal defect (VSD), patent ductus arteriosus (PDA), atrioventricular (AV) septal defect, etc. Total pulmonary to systemic blood flow ratios (Qp/Qs) determine the severity of symptoms.
Shunting with Right Ventricular (RV) Obstructive Lesions
Tetralogy of Fallot (TOF), Ebstein’s anomaly, and pulmonary valve (PV) stenosis with ASD or VSD constitute this category of shunts with limitation to pulmonary blood flow. The severity of obstruction determines the necessity of a patent PDA for pulmonary flow. The amount of hypoplasia of the pulmonary artery (PA) branches and the severity of elevated pulmonary vascular resistance (PVR) determine the level of cyanosis preoperatively.
Parallel Circulation
d-Transposition of the great arteries (d-TGA) is a prime example of parallel circulation where there is atrioventricular concordance and ventricular-arterial discordance. Balloon atrial septostomy may be warranted after birth for optimal intercirculatory mixing in the presence of an intact ventricular septum and a restrictive patent foramen ovale. In an uncomplicated d-TGA with intact ventricular septum and unrestrictive PFO, the pulmonary blood flow pattern is similar to that of a newborn with large ASD.
Single-Ventricle Lesions
This category includes defects such as single ventricle with obstruction to systemic flow (hypoplastic left heart syndrome, HLHS), single ventricle with obstruction to pulmonary flow (tricuspid atresia), single ventricle with common atrioventricular valve including heterotaxy variants and double-inlet single ventricle. A common feature essential for survival at birth is complete mixing of the oxygenated and deoxygenated blood at atrial and/or ventricular levels and patency of the PDA for effective systemic or pulmonary circulation. Strategies to manipulate Qp/Qs ratio are the mainstay of perioperative management by the anesthesiologist.
Left Ventricular Obstructive Lesions
Neonatal mitral stenosis, neonatal aortic stenosis, coarctation of the aorta, or a combination of the above resulting in Shone’s syndrome comprises of the anomalies presenting in the neonatal period. A left ventricular pressure overload with elevated left ventricular end-diastolic pressure is seen from aortic lesions. Pulmonary hypertension (PHTN) worsens when there is critical mitral valve stenosis from associated left atrial hypertension. Critical lesions require patency of PDA. Administering anesthesia and mechanical ventilation to children with critical left heart lesions requires cautious observation of the pulmonary vascular resistance (PVR) as a decrease in PVR after induction may dramatically alter the ratio of Qp:Qs resulting in rapid systemic hyoperfusion.
Mixing Lesions with Series Circulation
Anomalies of pulmonary venous return (total or partial) are diagnosed in the neonatal period. Obstructive TAPVR often presents as a surgical emergency with profound metabolic derangements, systemic hypoperfusion and requires careful ventilator and hemodynamic management as PVR remains hyperreactive, labile and often elevated pre- and post- repair.
Surgical Techniques
Surgical techniques for neonatal congenital heart lesions involve exposure to extreme conditions, for example, significant hemodilution with CPB, antegrade cerebral perfusion (ACP), and deep hypothermia with cardiac arrest. Individual techniques for each lesion are mentioned in different chapters of this book. An intraoperative management plan discussed with the cardiac surgical team stratifying the level of coordination and anticipating changes in physiology on termination of bypass is often required for optimal weaning from bypass.
Preparation for Anesthesia
The neonate’s birth details, clinical condition, review of the medical record, echocardiogram, and other diagnostic imaging and laboratory data needs to be discussed extensively with the pediatric cardiac team prior to the anesthetic. If the neonate is already intubated and mechanically ventilated, a review of respiratory mechanics, oxygenation status and trend of blood gas analysis is indicated. The operating room or catheterization laboratory needs to be warmed and a forced warm air blanket should be available. Anesthesia machine, back up neonatal ventilator, and monitoring equipment should be verified to be in perfect working order. Airway management instruments and endotracheal tubes in appropriate sizes should be available. All anesthesia and resuscitation drugs should be carefully drawn in appropriate size syringes and clearly labeled. Neonates usually arrive to the operating room with intravenous (IV) access and multiple infusions (total parenteral nutrition, lipids, prostaglandin E1 (PGE1), inotropic infusions, etc.); a careful evaluation and untangling of this network is warranted before anesthetic induction. Accidental flush of a PGE1-carrying IV lumen could result in significant hypotension and hemodynamic collapse.
Neonatal Airway Management
The true incidence of difficult airway (cannot ventilate, cannot intubate) is low in neonates except in syndromic children.5 A careful preoperative evaluation to assess for structural airway defects, such as cleft lip, cleft palate, mandibular hypoplasia, etc. helps in identifying predictors of a difficult airway. If there is a congenital airway lesion, for example, tracheo-esophageal fistula in a patient with CHD, the airway lesion may need to be corrected before the child is subjected to heart surgery.
Debate on the use of cuffed versus uncuffed ETs in neonates continue. Although uncuffed ETs have been the mainstay of care for neonates in the operating room and intensive care units, recent introduction of microcuff endotrachial tubes has apparently tipped the balance in favor of cuffed endotrachial tubes, although their long-term safety is still questioned.6
Uncuffed endotrachial tubes offer a larger size, ease of suctioning, and lower resistance for spontaneous ventilation. Drawbacks include inaccurate measurements of tidal volume and anesthetic gases, waste of inhaled gas with increased cost, and operating room pollution.7 Pediatric microcuff endotrachial tubes have a cuff that is located at the distal end of the endotrachial tube and is made out of ultra-thin polyurethane. This allows the microcuff to create an effective seal, accurately measure respiratory mechanics and retain the ability to measure a cuff pressure, and helps minimize the mucosal damage.6 The use of the microcuff endotrachial tube needs strict adherence to manufacturer’s guidelines, assurance of a leak with the cuff inflated and frequent cuff pressure measurements.
Anesthetic Management of the Neonate
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree