An Integrative Behavioral Approach for Adopting a Healthy Lifestyle After the Diagnosis of Heart Disease
Alan Rozanski
John is a 53-year-old lawyer and father of two teenage girls. Recently, John has experienced arm pain on a number of occasions while driving his car. His father had died of a heart attack at the age of 57. Concerned that his symptoms may represent heart disease, John makes an appointment to see a cardiologist. On physical examination, John is found to have normal findings except for mild elevation in his blood pressure and excess weight. He is 5 feet 8 inches and weighs 190 pounds. His resting electrocardiogram is normal. Because of the concern for heart disease, his physician orders blood work and a coronary artery calcium scan. The latter is ordered to assess if there is direct evidence of any atherosclerotic build-up in John’s coronary arteries. John’s blood work reveals an elevated cholesterol level and a borderline elevation in his blood sugar level. His coronary calcium score is substantial elevated (score of 620), thus indicating the presence of extensive underlying atherosclerosis in John’s coronary arteries. A stress test is subsequently ordered. The test reveals that John is quite deconditioned but as the test is normal, John’s physician informs him that consideration of a coronary stent placement or bypass surgery is currently not necessary. However, he advises John that it is important that he now work to control his risk factors for heart disease. Motivated by his newly discovered risk, John tells his physician he wants to do “whatever it takes.” John is placed on blood pressure and cholesterol-lowering medication and is told to go on a heart-healthy weight loss diet and to start exercising. In the past, however, John has not been successful in initiating a better diet and exercise and even sometimes forgets to take prescribed medications. Now that John is at risk, how can he be assisted in doing “whatever it takes”?
Heart disease is the most common chronic disease and the leading cause of death in the United States and other industrialized countries. Each year, >800,000 people die from heart disease in the United States and >1.2 million have either a new or recurrent heart attack. Since the 1960s, major risk factors for heart disease have been identified. The ones most commonly assessed and targeted for treatment include high blood pressure, high cholesterol, diabetes, smoking, obesity, and lack of exercise. The treatment of cardiac risk factors can slow the progression of heart disease and decrease the possibility of heart attack or fatal cardiac events.
It is often hard for people to fully adopt the lifestyles that can help prevent the progression of heart disease. Some patients become highly motivated to change their diet and start exercising after a heart attack, but then wane in their enthusiasm for maintaining their new health habits over time. Many other patients succeed in taking medications to control risk factors for heart disease but do not succeed in initiating behaviors that require a frank change in lifestyle. A surprising number of patients even find it difficult to just take the medications that have been ordered by their physicians.1
Generally people need guidance and help in adopting healthier lifestyles after the diagnosis of heart disease. Accordingly, this chapter will serve as a primer for physicians and patients alike regarding the full context of behavioral changes that can be adopted to promote a healthier lifestyle.
RISK FACTORS FOR HEART DISEASE
Besides the traditional behavior risk factors for heart disease (poor diet, lack of exercise, and smoking), over time a wide variety of other behaviors and psychosocial factors have been linked to the development of heart disease. These factors are listed in Table 38.1 and discussed below.
LACK OF ADEQUATE REST AND RELAXATION
The importance of rest and relaxation is being increasingly studied by physicians. A large category in this domain is sleep problems, which can be divided into three principal forms: (1) sleep apnea and other forms of sleep disordered breathing problems; (2) chronic insomnia; and (3) a voluntary restriction of sleep time. Both sleep apnea and insomnia can adversely affect health but the medical effects of undue voluntary sleep loss have only been recently delineated. Experimental work indicates that when volunteers are asked to curtail their sleep by 2 hours per night, a stress response is elicited in the body, consisting of diminished insulin sensitivity, increase in evening cortisol levels, and production of inflammatory proteins.2,3 In addition, short sleep has been linked to increase in appetite and weight. In part, this effect is due to a reduction in the secretion of an appetite suppressing hormone called leptin and an increase in an appetite stimulating hormone called ghrelin as people get less sleep.4 Recent epidemiologic data now also link short sleep to adverse clinical events.5,6 These results are of increasing interest because our society as a whole obtains less sleep than yesteryear. In 1960, the mean sleep time for Americans averaged around 8 hours per night but currently only averages approximately 6.5 hours per night.
TABLE 38.1 Spectrum of Behavioral Risk Factors for Heart Disease | ||
|---|---|---|
|
Difficulty in unwinding is also an increasingly studied area that has become more relevant as modern technology makes it possible and often routine for individuals to continue work after hours. Although more study is needed, a series of studies have now demonstrated an increase in clinical events among individuals who report difficulty in unwinding after work.7,8 Difficulty in unwinding after work may be physical or psychological in nature. Physically impaired unwinding is most commonly because of continued involvement in work on nights and weekends or demanding domestic duties after work. Psychologically impaired unwinding may be due to physiological arousal resulting from undue worry or rumination about work or other matters after leaving one’s job.
CHRONIC STRESS
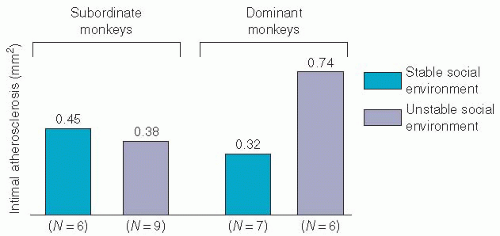
Modern medical science has identified the presence of a strong link between chronic stress and heart disease. Chronic stress is unique among psychosocial stresses because it can be easily produced and well quantified in animals. An important animal species in this regard is cynomolgus monkeys. This is because these animals develop atherosclerosis in a manner that is similar to humans. The experimental production of stress in such monkeys is based on their social tendencies.9 Specifically, when male monkeys are placed into a new group, they fight with each other until a pecking order from most dominant to submissive monkeys has been established. A stable order then ensues. However, if male monkeys are regrouped into new groups every few months, a situation of chronic stress is established (Figure 38.1). Male dominant monkeys who live under such stress are found upon necropsy to have substantially more atherosclerosis than their submissive counterparts or males that live in stable social groups9 (Figure 38.2).
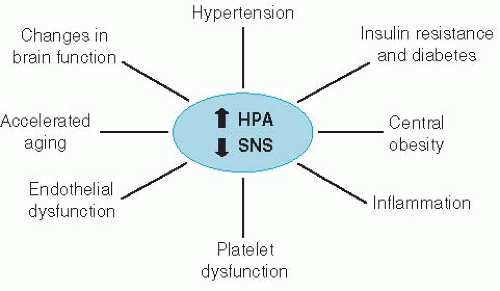
Over time, the mechanisms that account for the increased risk for atherosclerosis under conditions of chronic stress has been identified (Figure 38.3). Chronic stress is associated with a continuously elevated stimulation of two central brain systems: the hypothalamic-pituitary-adrenocortical (HPA) axis and the sympathetic nervous system (SNS) system.10 This stimulation results in elevated secretion of two “stress hormones”: cortisol and norepinephrine. Such chronic hormonal elevations are highly detrimental to health, resulting in metabolic abnormalities that favor the development of hypertension,11 insulin resistance (a precursor to diabetes),12 increased storage of fat in the abdomen,13 elevation in inflammatory proteins within the body,14,15 a tendency to increased coagulabilty of the blood,16 and a pathologic state of the inner lining of blood vessels (the “endothelium”) that prevents these blood vessels from properly vasodilating during periods of stress (a condition termed
“endothelial dysfunction”).17 Chronic stress can also promote ovarian dysfunction.18
“endothelial dysfunction”).17 Chronic stress can also promote ovarian dysfunction.18
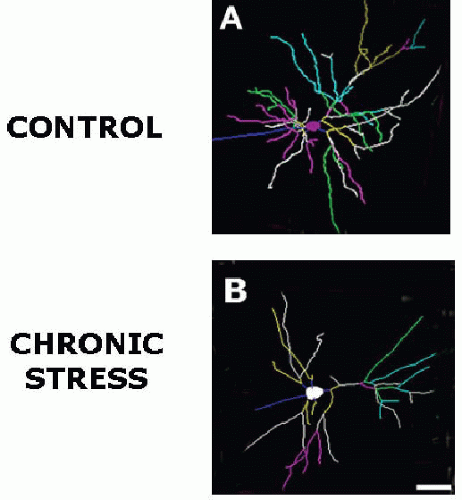
Among other effects, people under chronic stress are more likely to become physiologic “hyperreactors,” meaning that there is a tendency for heart rate and blood pressure responses to rise higher and recover more slowly following acute stimulations compared with people who are not under stress.19 More recently, Epel et al.20 have demonstrated that people under chronic stress are more likely to suffer from DNA evidence of accelerated aging, and McEwen21 demonstrated that chronic stress can cause adverse remodeling of the brain: an increase in size of the amgydala (the brain’s fear center), and reduction in the size of the hippocampus (involved in regulating long-term memory and other functions) and the prefrontal cortical regions of the brain (regulating “executive functions”) (Figure 38.4).
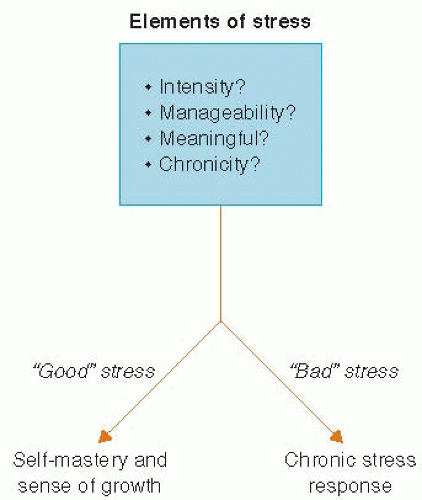
Many forms of chronic stress have been documented to cause heart disease and/or reduce longevity, including work stress, marital strain, and caregiver stress. However, in understanding stress, it is important to distinguish between stress that is “good” and “bad.” As depicted in Figure 38.5, whether a given life challenge is viewed as “good” or “bad” may depend on a number of factors, including the intensity of the stress, how manageable or controllable it is, how meaningful the stress experience is relative to one’s value systems and the chronicity of stress. For example, two people having the same amount of challenge in providing caregiving for an incapacitated elderly person may experience the challenge quite differently according to whether they find the experience to be personally meaningful or not. The more worthwhile the caregiving is viewed, the less likely there is to be early burnout.
When stress is well handled, it builds people’s coping skills, sense of self-mastery, and self-esteem. By contrast, as stress becomes more uncontrollable and prolonged, there is increasing likelihood that the chronic stress response that is outlined in Figure 38.3 will ensue.
CHRONICALLY NEGATIVE THOUGHT PATTERNS AND EMOTIONS
The presence of chronic negative emotions—chronic depression and chronic anxiety in particular and chronic negative thought patterns such as worry, hostility, and pessimism are health-damaging. Depression has been the most studied of the common negative emotional states. Depressive orders can vary from mild to severe. Major depression—characterized by a severely depressed mood, loss of interest, or pleasure in most activities, and somatic symptoms such as fatigue and insomnia—is a particularly disabling disorder that at any one time is present in approximately 5% of Americans. By contrast, major depression is consistently noted in approximately 15% of cardiac patient populations and another 15% have lesser but still concerning depressive symptoms.10 Thus, nearly one-third of cardiac patients have some level of depressive symptoms. This association is due to a bidirectional relationship between depression and heart disease: depression is a direct causative risk factor for heart disease but chronic illnesses such as heart disease can also help precipitate or worsen depressive symptoms in some patients. Study indicates a gradient relationship between the magnitude of depressive symptoms and the risk for adverse clinical outcomes (Figure 38.6).22
The mechanisms by which chronic depression causes heart disease is not dissimilar to mechanism by which chronic stress causes disease, but some difference in mechanisms is present. Like chronic stress, chronic depression is associated with high cortisol and norepinephrine secretion, resulting in insulin resistance and a threefold increased risk for diabetes, the development of abdominal obesity, elevation in inflammatory proteins, the development of platelet dysfunction, and presence of endothelial dysfunction.23,24,25,26,27,28 and 29 These changes combine to accelerate the development and progression of atherosclerosis. In addition, female patients experiencing chronic depression are at increased risk for developing osteoporosis30,31 (Figure 38.7). Thus, it is not surprising that epidemiologic study indicates that chronic depression is as potent as hypertension, diabetes, smoking, and other CAD risk factors in promoting heart disease.19
Anxiety syndromes that have now been strongly linked to heart disease include general anxiety disorder,32 phobic anxiety,33 panic disorder,34 and posttraumatic stress disorder.35 Another commonly studied negative thought-emotion complex that has been linked to heart disease has been chronic anger and/or hostility.36 More recently, there has been consistent study demonstrating the negative health effects of pessimism.37,38,39 and 40 In addition, pending further study, chronic worry,41 rumination,42 and even perfectionism43,44 are additional factors that have been preliminary linked to either a heightened frequency of clinical disease or to disturbances in the normal functioning of human physiology.
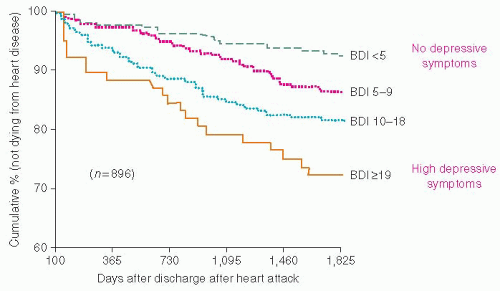 Figure 38.6. After sustaining a heart attack, 896 patients were assessed for the presence of depressive symptoms and then followed up for 5 years (1,825 days). Depression was measured by a questionnaire, the Beck Depression Inventory (BDI), with low scores (<5) indicating that no depressive symptoms were present. Progressively higher BDI scores are indicative of increasing depression. The vertical axis indicates the percent of patients who did not
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|