Chapter 9 Ambulatory Phlebectomy
Historical Background
Ambulatory phlebectomy (AP) is a minor surgical procedure designed to remove varicose vein clusters located close to the skin surface. Originally performed in ancient Rome, the technique was published by Robert Muller in 1966.1 In many office-based venous surgery practices in the United States, AP is performed with the use of local tumescent anesthesia. The six basic features of the technique are as follows:
Etiology and Natural History of Disease
Bulging varicose veins on the surface of the skin can originate from different sources. Identification of these sources is important because the source influences the treatment plan. Varicosities on the medial aspect of the thigh and calf are usually the result of great saphenous vein (GSV) incompetence. To minimize the chance for recurrence, the incompetent GSV must be eliminated from the circulation. This concept has been substantiated in several prospective randomized clinical trials involving patients who were treated with or without saphenectomy by conventional vein stripping.2–5 The recurrence rates for limbs without saphenectomy were much higher than those for limbs with saphenectomy. Of course, now thermal ablation techniques with either radiofrequency or laser have proved to be the methods of choice for eliminating the GSV from the circulation.6,7
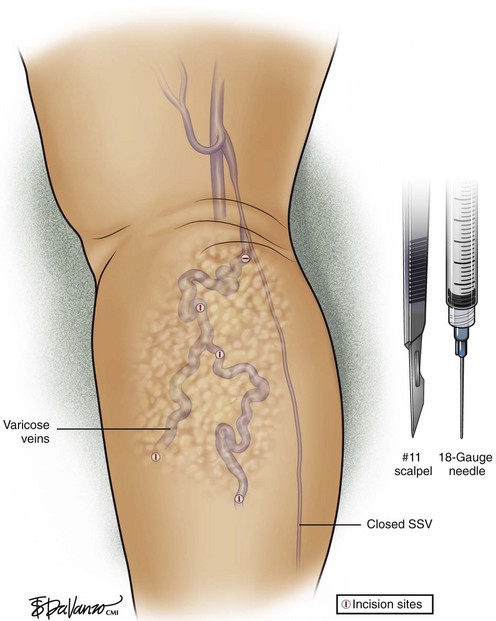
In cases where no “feeding source” is found, phlebectomy of the varicosities may be all that is required. Labropoulos et al.8 have shown that varicose veins may result from a primary vein wall defect and that reflux may be confined to superficial tributaries throughout the lower limb. Without great and small saphenous trunk incompetence, perforator and deep vein incompetence, or proximal obstruction, their data suggest that reflux can develop in any vein without an apparent feeding source. This is often the case when bulging reticular veins are seen along the course of the lateral leg. This lateral subdermic complex and its vein of Albanese are often dilated and bulging in elderly patients. The underlying source of venous hypertension is usually perigeniculate perforating veins, not easily identifiable with duplex imaging. AP using an 18-gauge needle stab incision and a small crochet hook for exteriorization of the vein is an excellent procedure for this clinical problem.
Imaging
We prefer mapping these veins using visual inspection and palpation; other investigators might prefer transillumination mapping using specialized vein lights.9 Ultrasound-guided vein hooking is useful for deeper veins.
Hemostasis and Anticoagulation
Klein10 has shown through clinical studies that a dose of 35 mg/kg of dilute lidocaine solution is well tolerated and safe. Infiltrating solutions should contain epinephrine in appropriate concentrations to induce vasoconstriction and more gradual absorption of lidocaine into the bloodstream.
Infections are rare after liposuction and venous procedures with tumescent anesthesia and are usually confined to the incision site.11 The reason for the low rate of infection is not clear, although there are reports of lidocaine concentration–dependent bacteriostatic and bactericidal activity. Pathogens commonly found on the skin may be sensitive to this activity.12
Operative Steps
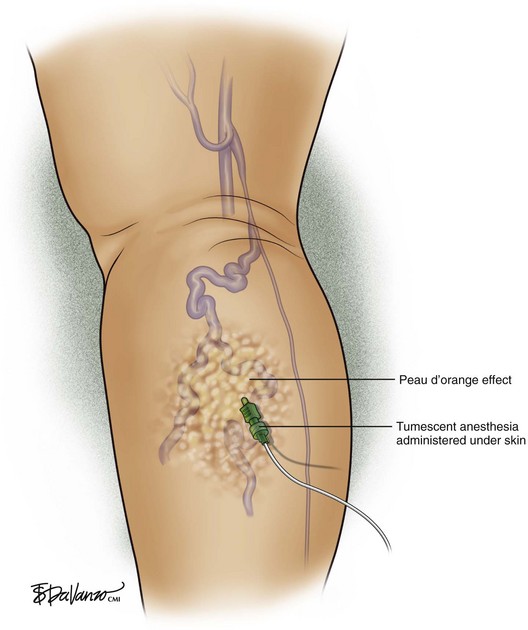
Tumescent anesthesia (Fig. 9-1): Tumescent anesthesia allows large areas of the body to be anesthetized with minimal effect on intravascular fluid status, avoidance of general anesthesia, and short postoperative recovery. Tumescent anesthesia provides a safe, easy-to-administer technique for use with AP. The technique of tumescent anesthesia involves infiltration of the subdermal compartment with generous volumes of a 0.1% solution of lidocaine with epinephrine. The anesthetic preparation is administered subdermally under pressure. The doctor pushes the fluid until a characteristic peau-d’orange effect is visualized on the skin. The tumescent fluid hydrodissects the subcutaneous fat from the venous tissue as it enters, thus facilitating vein extraction afterward.
Incisions (Figs. 9-2 and 9-3): The most popular instruments for creating incisions are No. 11 scalpel blades, 18-gauge needles, and 15-degree ophthalmologic Beaver blades. Incision length should correspond to vein size but is usually in the range of 1 to 3 mm. The author removes small varicose veins through an 18-gauge needle hole, while larger veins require slightly larger incisions made with a No. 11 scalpel blade.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree