Alternative Open Treatment of Renal Artery Occlusive Disease
James C. Stanley
Activation of the renin-angiotensin system and development of renovascular hypertension is a universal response to altered renal blood flow as a consequence of both arteriosclerotic and fibrodysplastic renal artery occlusive disease. Clinical manifestations of renovascular hypertension in children and adults have been well established, and diagnostic studies will confirm the presence of this disease in 80% to 95% of patients.
Conventional bypass procedures or endarterectomy may be hazardous in patients having compromised ventricular function and in whom aortic occlusion could precipitate a cardiac event. Similar procedures may prove unsafe in those having a severely diseased aorta or hostile retroperitoneum. Endovascular interventions are an increasingly successful means of managing patients in these circumstances, yet certain lesions will still require open surgical repair. In these high-risk settings, alternative therapies should be considered, including splenorenal, hepatorenal, iliorenal, and mesorenal bypasses.
Adequate exposure is an essential element for successful performance of alternative renal artery reconstructions. A transverse supraumbilical abdominal incision extending from the opposite midclavicular line to the posterior-axillary line on the side of the renal artery reconstruction (Fig. 41-1) offers a distinct technical advantage in the greater ease of handling instruments parallel to the longitudinal axis of the renal artery during complex procedures, and it provides easy access to the splenic, hepatic, superior mesenteric, or iliac arteries. Exposure is facilitated by placing a rolled pack under the lumbar spine to accentuate the patient’s lumbar lordosis. A midline vertical incision is favored by some surgeons. After the peritoneal cavity has been entered, the small intestines are retracted to the opposite side of the abdomen. In small adults, children, and infants, exposure of the renal vasculature is more easily obtained if the small intestines are displaced outside the confines of the abdominal cavity. Containment of the viscera in a plastic bag avoids organ desiccation and heat loss.
Splenorenal Bypass
Splenorenal bypass is a frequently performed alternative to an aortorenal bypass or endarterectomy for patients with left-sided disease. This usually involves direct end-to-end anastomosis of the splenic artery to the renal artery (Fig. 41-2). It is critical that pre-operative lateral aortography confirms that a significant celiac artery stenosis does not exist in these circumstances. Occasionally, this type reconstruction may necessitate placement of an interposition vein graft between the splenic and renal arteries.
The left renal artery is exposed by medial reflection of the left colon, distal duodenum, and pancreas. This approach is initiated by incising the lateral parities adjacent to the descending colon, followed by blunt finger dissection within the relatively avascular retroperitoneal tissues overlying the kidney and great vessels. As the dissection continues medially, the pancreas is elevated and retracted superiorly. Mobilization of the spleen may be required to prevent undue tension on its renal and lateral parietal attachments that might otherwise result in capsular or parenchymal tears. Fixed retractors are favored to displace these structures from the operative field. This extraperitoneal approach is preferred over exposure gained directly through an incision in the posterior retroperitoneum at the root of the mesocolon and mesentery.
Exposure of the left renal artery is facilitated by mobilization of the overlying renal vein with ligation and transaction of its gonadal and adrenal branches. The renal vein is usually encircled with an elastic vesselloop and retracted in an effort to better visualize the underlying artery. The renal artery should be freed from surrounding structures for 3 or 4 cm in order to allow the vessel to assume a gentle curve upward when anastomosed to the splenic artery.
The splenic artery can be palpated as it courses along the superior border of the pancreas a few centimeters above and in front of the left renal artery. Dissection of the splenic artery often requires ligation of its multiple small branches entering the pancreas. Tortuosity and calcification may make it difficult to mobilize the splenic artery for the anastomosis to the renal artery without buckling or kinking. Because of the latter, care in positioning the splenic artery before completing an anastomosis to the renal artery is very important to ensure a good technical result. This mandates an early recognition of the reconstruction’s posterior location when the pancreas and foregut structures are returned to their usual place within the abdomen.
The splenic and renal arteries, or an interposition vein graft if used, should be spatulated on opposite sides in order to create a generous ovoid end-to-end anastomosis. Although some report end-to-side, splenic artery-to-renal artery reconstructions when significant size differences in these two arteries exist, this manner of anastomosis is not favored. Splenorenal bypasses in children
are also not favored, because of early vasospasm-related thromboses, as well as late problems if celiac artery stenotic disease evolves as the child grows into adulthood. The latter is known to result in recurrent hypertension in these younger patients.
are also not favored, because of early vasospasm-related thromboses, as well as late problems if celiac artery stenotic disease evolves as the child grows into adulthood. The latter is known to result in recurrent hypertension in these younger patients.
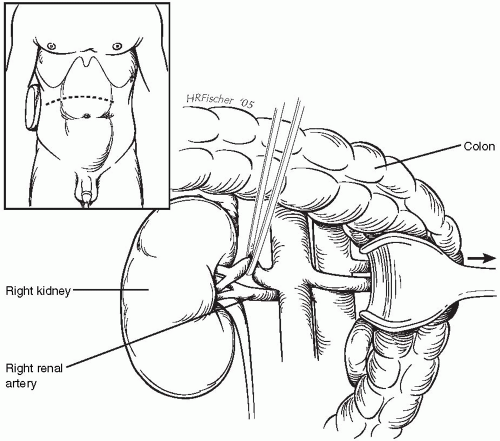 Figure 41-1. Operative approach to the right renal artery, using a transverse, supraumbilical incision with an extraperitoneal dissection and retraction of the colon and foregut structures medially. |
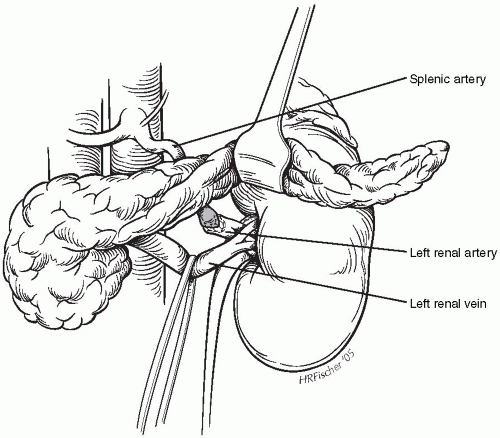 Figure 41-2. Splenorenal bypass following mobilization of the splenic artery, with an end-to-end anastomosis to the transected left renal artery. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


