Alternative, Open Revascularization for Aortoiliac Occlusive Disease
Alexander D. Shepard
Mark F. Conrad
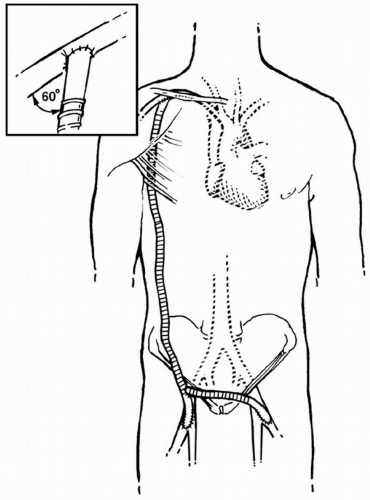
Aortobifemoral bypass remains the operative treatment of choice for patients with aortoiliac occlusive disease because of its superb long-term durability and effectiveness. However, aortofemoral grafting is not an appropriate choice in some patients because of unacceptable medical risk factors and/or anticipated technical difficulties. Alternative, open approaches to aortoiliac reconstruction in such patients usually involve extra-anatomic bypasses, which are chosen to avoid the risks associated with opening the abdomen and/or cross-clamping the aorta. Femorofemoral and axillofemoral bypass are the procedures most frequently used in these situations, but they should be considered compromise operations.
Femorofemoral Bypass
Since its introduction more than 40 years ago, femorofemoral bypass has remained the most widely used procedure for the treatment of symptomatic unilateral iliac artery occlusive disease that is not amenable to angioplasty or stenting. The simplicity and low morbidity and mortality of this procedure have made it quite popular. Many early reports documented patency rates that were nearly equivalent to aortofemoral bypass, which led some authorities to use this procedure even in good-risk patients. Several series over the past decade, however, have questioned the long-term durability of this bypass, suggesting that its use should be limited to high-risk patients or those with technical contraindications to aortofemoral grafting.
Indications and Contraindications
Indications for femorofemoral bypass include disabling claudication or critical limb ischemia secondary to significant unilateral iliac artery occlusive disease with minimal or no disease in the contralateral iliac system. The procedure can also be used in the settings of iliac artery trauma necessitating ligation in a contaminated or scarred operative field, iatrogenic injury (postcatheterization or following placement of an intra-aortic balloon pump), or aortic dissection involving only one iliac artery. Further indications include an occluded limb of an aortobifemoral bypass that cannot be opened, an infected iliac artery aneurysm, or in combination with an aorto-uniliac endoluminal graft in the treatment of some abdominal aortic aneurysms (AAAs). Femorofemoral bypass is most commonly used in patients with unilateral common iliac disease that is not amenable to percutaneous intervention (i.e., angioplasty with or without stenting). In patients with isolated external iliac disease, iliofemoral bypass may be a better option, or rarely, endarterectomy may be a better option.
Because of the limited long-term patency of femorofemoral grafts, we reserve this bypass for patients at higher surgical risk with predictably low survival and for patients with severe, acute ischemia who cannot undergo appropriate pre-operative evaluation and preparation. In good-risk patients with a reasonable life expectancy, a direct aortic reconstruction (i.e., aortobifemoral bypass) is preferred, particularly if they have any occlusive disease of the aorta or donor iliac artery or if the indication for operation is lifestyle-limiting claudication. Femorofemoral bypass potentially places both lower extremities at risk to improve the perfusion of one and can render future femoral access (e.g., for cardiac catheterization) problematic.
Pre-operative Assessment
The aorta and donor iliac artery must be carefully evaluated pre-operatively. The symptomatic limb should have a weak or absent femoral pulse, while the donor limb should have a normal femoral pulse. A triphasic femoral artery waveform and/or a normal high thigh pressure by segmental limb pressure measurements are usually sufficient proof that the donor iliac system is relatively disease-free. Aortography with runoff views to at least the level of the tibial vessels is performed to define the presence, location, and severity of occlusive lesions. Bilateral oblique views of the pelvis are necessary to fully assess the iliac arteries, because posterior plaque is frequently present and may be missed on standard anterior-posterior views. The femoral bifurcations should also be carefully studied to detect disease at the origins of the profunda femoris arteries that may require correction at the time of bypass. If there is any question about the hemodynamic significance of a visualized iliac stenosis, intra-arterial pressure measurements proximal and distal to the lesion should be obtained. Any pressure gradient at rest is considered significant and can be confirmed by repeating the distal pressure measurements after provocative testing;
we prefer intra-arterial infusion of a vasodilator, such as papaverine. Such testing may be necessary to confirm the suitability of a diseased-appearing iliac as a “donor” artery for a more diseased contralateral iliac system. If a discrete, hemodynamically significant iliac stenosis is detected on the donor side, it can be treated with angioplasty/stenting to allow performance of a femorofemoral bypass in a high-risk patient who is not a good candidate for aortofemoral grafting. Several studies have documented that donor iliac artery angioplasty does not negatively impact the long-term outcome of femorofemoral bypass. Donor and recipient femoral artery disease can and should be corrected at the time of operation.
we prefer intra-arterial infusion of a vasodilator, such as papaverine. Such testing may be necessary to confirm the suitability of a diseased-appearing iliac as a “donor” artery for a more diseased contralateral iliac system. If a discrete, hemodynamically significant iliac stenosis is detected on the donor side, it can be treated with angioplasty/stenting to allow performance of a femorofemoral bypass in a high-risk patient who is not a good candidate for aortofemoral grafting. Several studies have documented that donor iliac artery angioplasty does not negatively impact the long-term outcome of femorofemoral bypass. Donor and recipient femoral artery disease can and should be corrected at the time of operation.
Patients undergoing femorofemoral bypass because of a perceived high operative risk should be carefully evaluated pre-operatively to ensure that they are indeed at high risk for an aortofemoral bypass. Over the past decade, we have successfully performed aortofemoral grafting on six patients presenting with occluded femorofemoral bypasses in whom the primary reason for their initial bypass was “prohibitive” operative risk. Young patients in particular warrant careful scrutiny.
Operative Technique
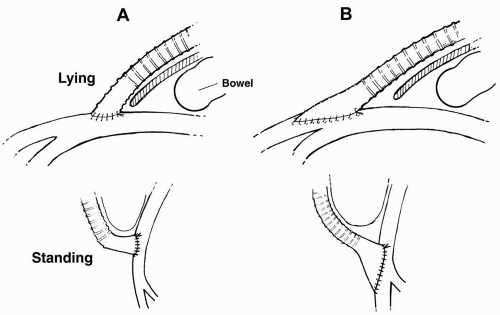
All patients should receive prophylactic antibiotics pre-operatively (usually a firstgeneration cephalosporin). We prefer epidural anesthesia, although a light general anesthesia is acceptable. In thin, high-risk, emergency patients, local anesthesia can be used. The entire abdomen and both groins to the mid thighs are prepped and draped. The femoral arteries are exposed through standard vertical groin incisions placed slightly more distally than normally, because there is frequently no need to divide the inguinal ligament. The inguinal ligament should be visualized at the uppermost extent of the incision, but otherwise it should be avoided to ensure that the anastomoses are placed far enough distally on the femoral arteries to avoid acute angulation of the graft as it courses out of the groins across the lower abdominal wall (Fig. 45-1). Care should be taken in exposing the femoral arteries to ligate crossing lymphatics, because any wound complication with a subcutaneously tunneled prosthetic graft can be catastrophic. The common femoral artery is exposed from the inguinal ligament to its bifurcation, and the origins of the superficial and deep femoral arteries are controlled as necessary to correct associated outflow disease.
A gently curved subcutaneous tunnel is created between the two groins across the lower abdominal wall (inverted “C” configuration) (Fig. 45-2). A large C-shaped aortic clamp or a tunneling device can be helpful. There is always some resistance in the midline where the skin is anchored to the fascia by a narrow band of connective tissue. Creating this tunnel after a lower midline incision can be problematic, and attention should be taken to avoid subfascial tunneling or inadvertent entry into the abdomen in such patients.
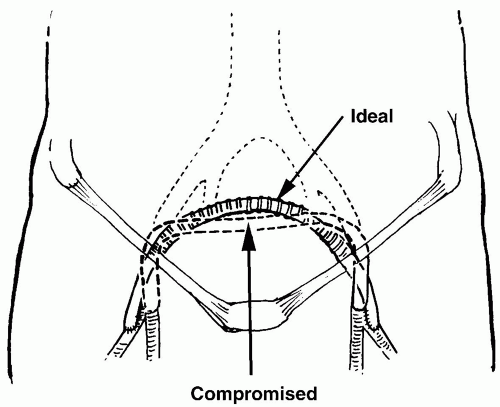 Figure 45-2. Configuration of femorofemoral graft showing tunnel and oblique groin anastomoses over origin of profunda femoris arteries. |
Great care should also be exercised in choosing the sites of graft origin and termination on the femoral arteries. The femoral artery immediately adjacent to the inguinal ligament should be avoided because of the potential for graft kinking as the abdomen “drops” or sags when the patient assumes an upright position (particularly in obese patients). For this reason, the femoral anastomoses are usually placed at the level of the bifurcations crossing over onto the origins of either the superficial or profunda femoris arteries; with high bifurcations it may
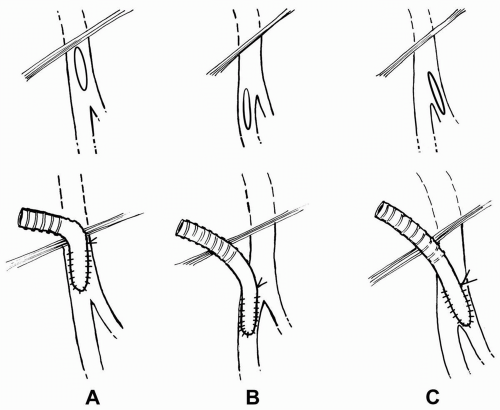
occasionally be necessary to place the anastomosis entirely on one of these femoral artery branches (Fig. 45-3A). Alternatively, the graft can be tunneled subfascially through the preperitoneal Retzius space. Oblique femoral arteriotomies carried down onto the profunda femoris arteries reduce the angle of graft curvature and correct any outflow disease present at the origin of the vessel (Fig. 45-3B). Inattention to these details of graft orientation and tunneling can lead to graft kinking and/or compression with thrombosis in the early postoperative period.
occasionally be necessary to place the anastomosis entirely on one of these femoral artery branches (Fig. 45-3A). Alternatively, the graft can be tunneled subfascially through the preperitoneal Retzius space. Oblique femoral arteriotomies carried down onto the profunda femoris arteries reduce the angle of graft curvature and correct any outflow disease present at the origin of the vessel (Fig. 45-3B). Inattention to these details of graft orientation and tunneling can lead to graft kinking and/or compression with thrombosis in the early postoperative period.
Removal of occlusive plaque within the donor femoral artery (and occasionally the distal external iliac artery) and the outflow tract of the recipient femoral artery is particularly important. If an extensive endarterectomy of the femoral artery/bifurcation is necessary, it is usually best to close the artery with a patch and sew the graft into the patch, rather than trying to cover the entire arteriotomy with the hood of the graft. Use of the latter technique frequently leads to graft kinking, as described above (Fig. 45-4). In the presence of superficial femoral artery occlusion on the recipient side, correction of profunda outflow disease is critical to the success of this procedure and may require an extended endarterectomy/profundaplasty. It is occasionally necessary (rarely in our experience) to combine a femoral-popliteal/distal bypass with a femorofemoral bypass. In this situation it is usually easiest to originate the distal graft from the hood of the femorofemoral graft, taking care to avoid angulation of the distal graft just beyond this proximal anastomosis.
We prefer to use a 7 or 8 mm (occasionally 6 mm with small arteries) externally supported polytetrafluoroethylene (PTFE) graft for femorofemoral grafting. However, a recent Veterans Affairs trial showed no advantage of PTFE over Dacron in this position. Supported grafts appear to be more resistant to kinking and compression than nonsupported grafts. Saphenous vein can be used when infection is a concern but can present problems because of their smaller caliber and increased risk of kinking. End-to-side anastomoses to the femoral arteries are constructed with 5-0 or 6-0 polypropylene or PTFE suture. If the common and superficial femoral arteries are occluded on the recipient side, an end-to-end anastomosis to the profunda can be performed. Meticulous wound closure is important to avoid wound complications that could prove catastrophic with a subcutaneously tunneled prosthetic graft.
Complications and Postoperative Management
Because of the extracavitary nature of this procedure, femorofemoral bypass is well tolerated even by high-risk patients. Mortality is low for elective procedures averaging 2% to 4% in most recent series. Major complication rates are equally low. Antiplatelet agents (we prefer aspirin) are started pre-operatively and continued postoperatively on a long-term basis. We frequently add dextran in the peri-operative period, avoiding it only in patients with significant left ventricular dysfunction or renal insufficiency. Patients are maintained on bedrest for 2 or 3 days postoperatively to minimize the risk of wound complications. In obese patients, particular attention is focused on groin hygiene. Ankle-brachial indices (ABIs) are checked in the early postoperative period to document a satisfactory hemodynamic result. Because progression of occlusive disease within the inflow and outflow circuits is the most common correctable cause of graft failure, patients are followed up at regular intervals in the outpatient clinic. Surveillance vascular laboratory testing includes ABIs and duplex scanning of the anastomotic sites.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree