INDICATIONS/CONTRAINDICATIONS
Airway stenting is used to treat obstructing lesions of the central airways, defined as the trachea, main bronchi, and the bronchus intermedius. Generally, lesions obstructing at the lobar or segmental level are not amenable to stenting due to lack of efficacy or functional benefit. Central airway obstruction can be caused by both benign or malignant etiologies, but the majority of patients suffer from malignancies, primarily direct involvement from bronchogenic carcinoma, or direct invasion from carcinomas of adjacent structures such as the esophagus or thyroid, but occasionally due to metastatic disease involving the airway directly, or indirectly from adjacent mediastinal lymph nodes. Most of these malignant lesions are surgically inoperable due to advanced stage disease and therefore the primary role of airway stenting in malignant disease is usually palliative. Airway stenting is infrequently performed because of surgical ineligibility due to inadequate physiological reserve in patients who might otherwise be candidates for resection. Airway stenting is nearly always combined with other bronchoscopic modalities for treating the endoluminal lesion, which can include (1) core-out and mechanical debridement; (2) airway dilation; (3) resection with different energy sources or cryotherapy; and (4) endoluminal brachytherapy or photodynamic therapy. The modalities chosen to treat the obstruction depend on the anatomy and characteristics of the obstruction, the training and experience of the thoracic surgeon or interventional pulmonologist, and the equipment available; however, lesions causing extrinsic airway compression and mixed lesions with a significant extraluminal component usually require stenting for adequate palliation of symptoms (Fig. 2.1).
Stenting should be considered when there is persistent symptomatic airway narrowing after other interventions such as core-out or dilatation, typically when the diameter of an affected airway remains <50% of normal diameter. Airway stenting should also be considered when there is central airway narrowing and external beam radiation treatment of the central airway is planned, in order to avoid anticipated greater significant airway narrowing that can occur subacutely with radiotherapy. Other indications for airway stenting due to malignant processes include management of airway fistulas.
Airway stenting for central airway obstruction due to benign etiologies should be approached cautiously and generally as a treatment of last resort when other, more definitive, or less invasive techniques are not successful. The most common benign cause of central airway obstruction occurs from postintubation stenosis; typically due to prolonged intubation. Other benign etiologies causing central airway obstruction include infectious and inflammatory processes such as tuberculosis, Wegener’s disease, relapsing polychondritis, fibrosing mediastinitis, and endobronchial papillomatosis. The thoracic surgeon should adhere to the basic principle of treating central airway obstructions caused by benign disorders with curative surgical resection if at all feasible. Patients with benign diseases are usually younger and expected to have longer life expectancies and the complications associated with prolonged airway stenting will often overshadow the palliative benefits. If airway stenting is necessary in patients with benign lesions, fully covered removable stents are required. One increasingly common indication of stenting for benign disease is airway stenoses following sleeve resections and bronchial anastomoses in lung transplant patients.
The primary contraindication for airway stenting is when surgical resection of the disorder causing the airway obstruction is possible. Therefore, it is imperative that an experienced thoracic surgeon evaluates a patient presenting with central airway obstruction before undergoing stenting or other endoscopic treatment. Although endoscopic management such as debridement and dilation may temporarily stabilize and palliate a patient with symptomatic central airway obstruction to evaluate for possible resection, airway stenting preceding a planned resection of the obstructed airway segment can create local inflammation and mucosal damage that may interfere with anastomotic healing following airway resection and reconstruction.
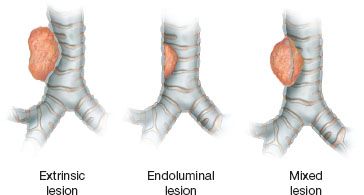
Figure 2.1 Lesions can cause tracheobronchial obstruction by extrinsic compression of the airway, endoluminal obstruction arising from the airway itself, or mixed lesions with both extrinsic and endoluminal obstruction.
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
Imaging
Patients with large airway obstruction are likely to present with dyspnea, stridor or wheezing, cough, and occasionally hemoptysis. Chest radiographs are universally obtained in patients with symptoms from airway obstruction and may be useful if the x-ray demonstrates a tracheobronchial mass or distortion of the tracheobronchial airway column. Also if pneumonia or postobstructive consolidation is evident, antibiotic therapy should be appropriately initiated. Neck and chest CT scans provide much better detail of airway and mediastinal anatomy, particularly with the higher resolution scanners that are readily available now at most facilities. Coronal and sagittal views, as well as the capability of generating three-dimensional (3D) reconstructions, provide excellent detail of airway anatomy that helps identify the location and extent of stenosis prior to bronchoscopy. These images can be useful for planning different therapeutic options, potential hazards, and the likelihood of successful intervention.
Choice of Stent
Stenting airway lesions require a thorough understanding of the various advantages and disadvantages of the available airway endoprostheses. The ideal endoprosthesis is a stent that is (1) easily deployed and adjusted but does not readily migrate; (2) resists compressive forces yet does not erode or breach the native airway mucosa; (3) conforms to the airway contour without kinking or bending; (4) elicits minimal foreign body reaction and prevents tissue ingrowth or granulation; and (5) allows mucociliary clearance to decrease mucous impaction. Unfortunately, the ideal airway endoprosthesis is not presently available. Current airway stents have some of these properties, but none have all.
TABLE 2.1 Common Commercially Available Tracheobronchial Stents
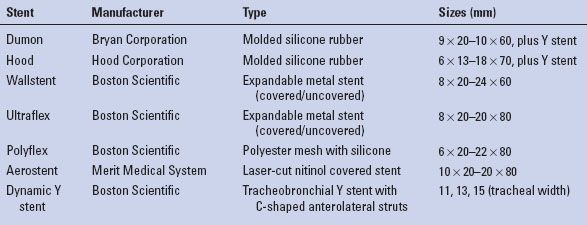
There are basically two main categories of airway stents: Silicone and metal, and selections from both categories should be readily available for deployment in any given clinical scenario. The main advantages of silicone stents are that they are inexpensive to manufacture; once positioned, easy to adjust and remove; and relatively well tolerated with minimal reactivity for granulation formation. These stents come in a variety of different diameters and different lengths (Table 2.1). The reported disadvantages of silicone stents are that they are stiff and more difficult to deploy, requiring general anesthesia, intubation, and skill with rigid bronchoscopy; although this in itself should not be a major limitation in the majority of patients. However, a considerable amount of sheer force may be required to push the stent across a tight stenosis or stricture, which can traumatize the airway. There are times that silicone stents may not generate sufficient radial force for some strictures or extrinsic compression from tumor. They also do not seat well in malacic segments or conform to longer tortuous stenotic segments and thus will commonly migrate from position causing itself airway obstruction. It is important to be aware that silicone stents can ignite with laser treatment, which often is used to treat airway granulation. Two types of molded silicone stents are commercially available, Dumon stents and Hood stents. Both are similar in characteristics, each with different versions of external studs or flanges for airway fixation (Fig. 2.2). The Hood and Dumon stents are essentially cylinderized versions of the Montgomery T-tube, a silicone-molded stent that is useful to consider in select patients who have a tracheostomy stoma or benefit from the additional stabilization of the T-limb, yet have a functional larynx.
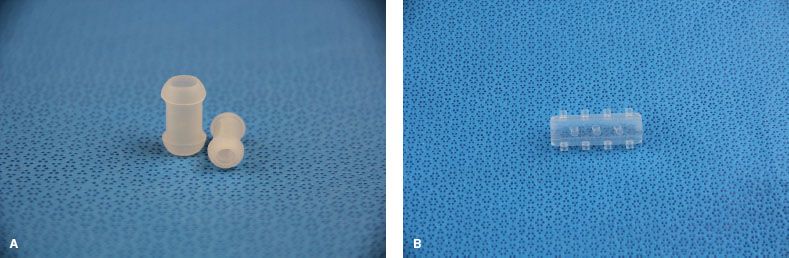
Figure 2.2 Molded silicone stents. A: Hood silicone stents and Dumon-style stents are similar. B: Dumon stents have studs.
Expandable bare metal airway stents have a more favorable inner luminal to outer luminal diameter ratio than silicone stents and are easier to deliver, using flexible bronchoscopy with or without fluoroscopy under topical or general anesthesia. Once delivered, these stents are extremely stable and there is low likelihood of dislodgment or migration. However, nearly all stents used today are covered metal stents that have some of the same potential for dislodgment as the solid silicone stents. The second-generation stents (e.g., Wallstent & Ultraflex stent) conform well to airway contours allowing greater adaptability for their use in more tortuous airway anatomy. Expandable metal stents can generate considerable radial force, which may be favored in fibrotic strictures. Uncovered metal stents theoretically allow mucosal neoepithelialization with the reported possibility to resume mucociliary clearance and also allow ventilation of lobar orifices across the open interstices. However, in reality this potential benefit is far overshadowed by tissue ingrowth and granulations through the interstices that frequently occurs due to the foreign body reaction to the stent. This often results in obstruction of the stent itself, yet once embedded in the airway wall the bare metal stents are extremely difficult to remove without causing significant secondary airway damage. Recurrent obstruction from tissue or tumor ingrowth through the metal interstices can require repeated debridement or even repeat stenting within the stent. Expandable stents also can exert considerable radial force and therefore, may erode through the airway into adjacent structures and risk creating a possible life-threatening bronchovascular fistula. As a result of these known shortcomings and complications, the US Food and Drug Administration (FDA) issued a warning that bare metal airway stents should be avoided in the management of benign airway stenosis.
The experience of airway interventionalists and the complications of bare expandable metal stents led to the development of third-generation–covered expandable metal stents. These stents are now widely available and used in the United States and internationally. One version of these stents is covered in the middle portion of the stent but bare at the ends. These are easier to adjust and remove than uncovered stents, but the metal ends of these stents are exposed and can become incorporated in the tracheobronchial mucosa from granulation and tissue overgrowth as well (Fig. 2.3). Yet more modern stents are fully covered, such as the Polyflex or Aero stents. The Polyflex self-expandable stent is composed of a polyester mesh with a silicone coating and does not have uncovered metal edges and therefore share advantages and disadvantages from both silicone and metal airway stents, while the Aero stent consists of a metal nitinol framework covered completely with polyurethane.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


