Adult Congenital Heart Disease
Luke J. Burchill
Adult Congenital Heart Disease Source Material
Published guidelines for the management of adult congenital heart disease (ACHD) patients provide an excellent overview of ACHD and are a rich source of questions for the cardiology boards.1–5 The questions in this section relate directly to existing guidelines for the care of ACHD patients, with particular emphasis given to the American Heart Association (AHA) guidelines.
QUESTIONS
1.A 55-year-old woman with a history of unrepaired ventricular septal defect (VSD) and Eisenmenger physiology presents to your clinic. Her most recent hemoglobin measured 17.5 g/dL (11.5 to 15.0), hematocrit 55% (36 to 46), mean corpuscular volume (MCV) 76 (83 to 99), and platelet count 140 × 103 cells/μL (150 to 400). She reports New York Heart Association class III limitations with increasing fatigue and infrequent headaches over the last 6 months. Blood pressure (BP) 110/70 mmHg, heart rate (HR) 70 BPM, and regular, O2 saturation 77% on room air. Cardiac examination reveals peripheral clubbing and cyanosis, a parasternal heave, loud P2, and a murmur of tricuspid regurgitation (TR). Electrocardiogram (ECG) shows sinus rhythm. She has had repeat phlebotomy for treatment of presumed hyperviscosity syndrome but does not feel any better. What of the following options is the most appropriate next step in management?
a.Phlebotomy should continue until symptoms improve.
b.Refer for heart–lung transplantation.
c.Measure serum erythropoietin.
d.Commence a pulmonary vasodilator.
e.Obtain iron studies.
2.A 25-year-old man presents to your clinic with 48-hour history of documented fever and chills. He has a history of a “hole in the heart” and examination reveals a 4/6 systolic murmur heard loudest at the lower left sternal edge. A restrictive muscular VSD is confirmed on echocardiogram. Which of the following is the most appropriate next step?
a.Oral antibiotics
b.Intravenous (IV) antibiotics
c.Blood cultures
d.Transesophageal echocardiogram
e.Cardiac surgery consult
3.Blood cultures are positive for Streptococcus viridans and the patient is treated for infective endocarditis (IE). A small mobile echodensity is noted adjacent to the VSD. At clinic review 3 months later he is much improved, repeat blood cultures are negative, and transesophageal echocardiography (TEE) is negative for vegetations. The patient asks whether his VSD should now be closed. What is the best answer?
a.Closure is indicated in those with a VSD complicated by IE.
b.VSD closure is NOT indicated in those with a VSD complicated by IE.
c.VSD closure is only indicated in the presence of a significant shunt (Qp/Qs, pulmonary to systemic blood flow ratio ≥2.0).
d.VSD closure is only indicated in the presence of a significant shunt accompanied by symptoms.
4.For which of the following conditions is IE prophylaxis not required prior to extensive dental procedures (more than one option may be correct)?
a.Ebstein anomaly without prior intervention
b.4 weeks following percutaneous closure of a secundum atrial septal defect (ASD)
c.Mechanical aortic valve replacement (AVR) for bicuspid aortic valve disease
d.Eisenmenger syndrome
e.Tetralogy of Fallot (TOF) with residual VSD at the site of prior surgical repair
5.With which of the following adult congenital heart conditions can the following ECG tracing be seen (Fig. 9.1)?
a.Primum ASD
b.Congenitally corrected transposition
c.Ebstein anomaly
d.VSD
e.Coarctation of the aorta
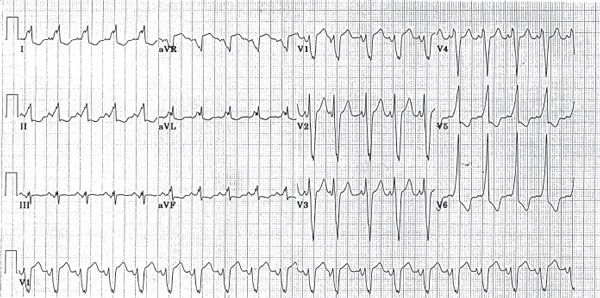
Figure 9.1
6.Which of the following is an absolute contraindication to pregnancy?
a.Surgically corrected transposition of great arteries
b.Congenitally corrected transposition of great arteries
c.Ebstein anomaly
d.Eisenmenger syndrome
e.Status post Fontan operation
Questions 7 to 11
Match the following conditions with their corresponding surgical procedures. There may be more than one answer for each question.
7.Pulmonary atresia
8.D-transposition of great vessels
9.Tricuspid atresia
10.Congenitally corrected transposition of the great arteries
11.Aortic stenosis
a.Ross
b.Blalock-Taussig
c.Senning or Mustard
d.Arterial switch
e.Fontan
f.Rashkind
g.None of the above
Questions 12 to 16
Match the following disease conditions with their gender preponderance.
12.VSD
13.ASD
14.Bicuspid aortic valve
15.Coarctation of the aorta
16.Pulmonary atresia with an intact ventricular septum
a.Predominantly male
b.Predominantly female
c.Equal preponderance
Questions 17 to 21
Match the following cardiac catheterization still-frame slides (Figs. 9.2, 9.3, 9.4, 9.5, and 9.6) to their respective diagnoses.
17.Figure 9.2
18.Figure 9.3
19.Figure 9.4
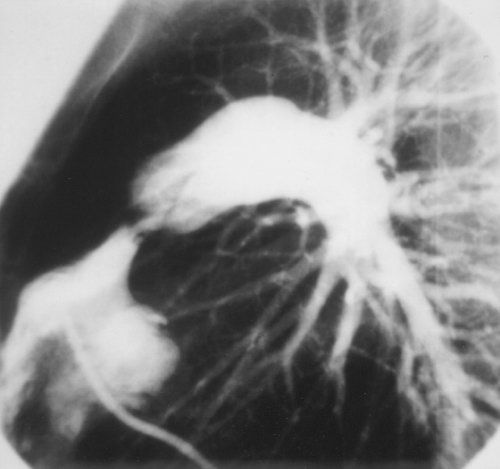
Figure 9.2

Figure 9.3
20.Figure 9.5
21.Figure 9.6
a.Coarctation of the aorta
b.Patent ductus arteriosus (PDA)
c.Hypertrophic cardiomyopathy
d.Pulmonic stenosis
e.VSD
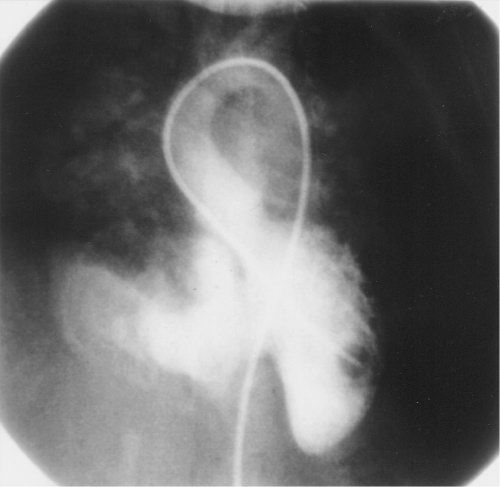
Figure 9.4

Questions 22 to 26
Match the physical examination findings with the corresponding adult congenital heart disorder.
22.Right ventricular (RV) lift with a loud systolic ejection murmur along the left sternal border, with a single S2
23.Systolic ejection click, loud S1, holosystolic murmur, split S2 and hepatomegaly
24.Weak or delayed femoral arterial pulses, harsh systolic ejection murmur in the back, and a systolic ejection click in the aortic area
25.Cyanosis, digital clubbing, loud P2, and a variable Graham Steell murmur
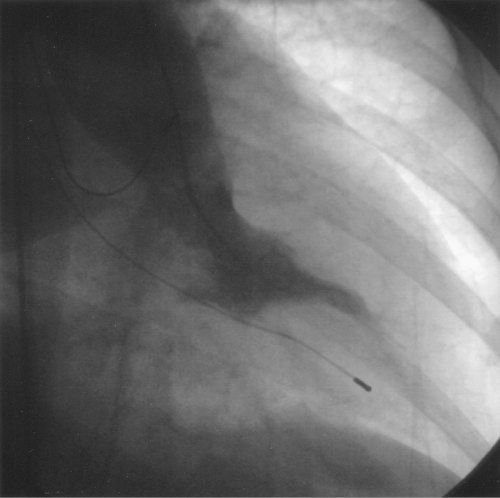
Figure 9.6
26.Wide pulse pressure, prominent left ventricular (LV) impulse, and a continuous machinery murmur enveloping S2
a.Eisenmenger syndrome
b.Coarctation of the aorta
c.PDA
d.Ebstein anomaly
e.TOF
Questions 27 to 31
Match the following congenital defects with their associated disease conditions. (more than one may apply)
27.Ostium primum ASD
28.Noonan syndrome
29.Coronary sinus ASD
30.Williams syndrome
31.Sinus venosus ASD
a.Supravalvular aortic stenosis
b.Supravalvular pulmonic stenosis
c.Cleft mitral valve
d.Anomalous pulmonary venous drainage
e.Persistent left superior vena cava (SVC)
Questions 32 to 36
Match the characteristic chest radiography findings with the corresponding congenital disorder.
32.Prominent central pulmonary arteries (PAs) (possible calcifications) and peripheral pruning
33.Right aortic arch, RV enlargement, and a “boot-shaped” heart
34.Marked cardiomegaly, severe right atrial (RA) enlargement, and normal lung fields
35.Posterior rib notching and a “reverse E” or “3” sign
36.Pulmonary plethora, prominent ascending aorta, proximal PA dilatation, and opacity at the confluence of the aortic knob and descending aorta
a.Eisenmenger syndrome
b.Coarctation of the aorta
c.PDA
d.Ebstein anomaly
e.TOF
Questions 37 to 41
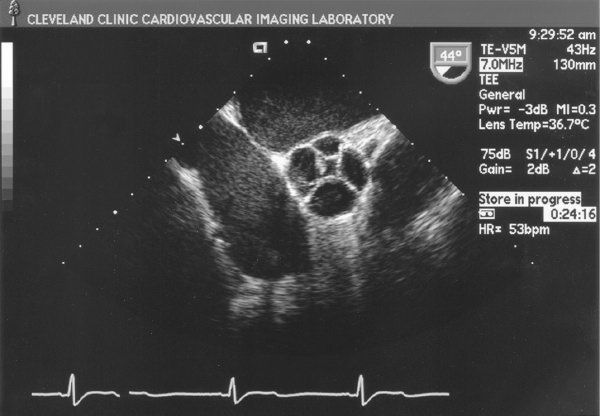
Match the following congenital cardiac disorder with the characteristic transthoracic echocardiogram (TTE) finding (Figs. 9.7, 9.8, 9.9, 9.10, and 9.11).
37.Bicuspid aortic valve
38.Cor triatriatum
39.Ostium primum ASD
40.Quadricuspid aortic valve
41.Subaortic valve stenosis
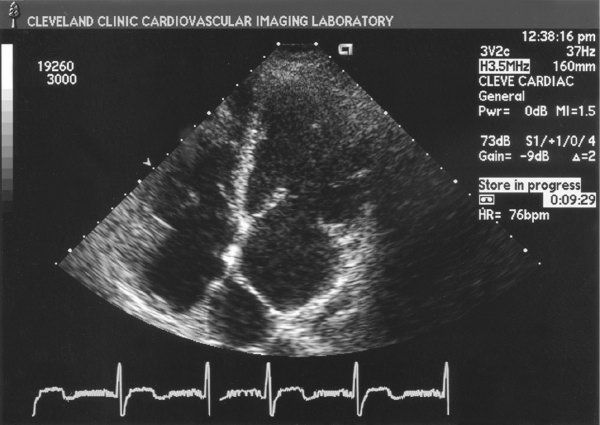
Figure 9.7
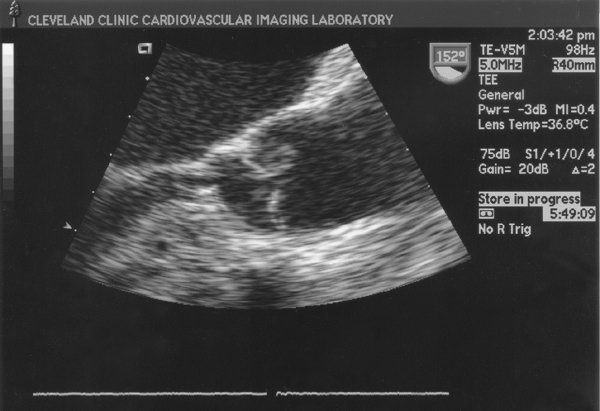
Figure 9.8
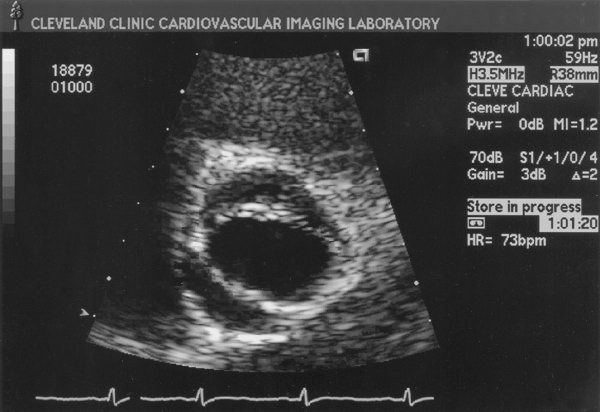
Figure 9.9
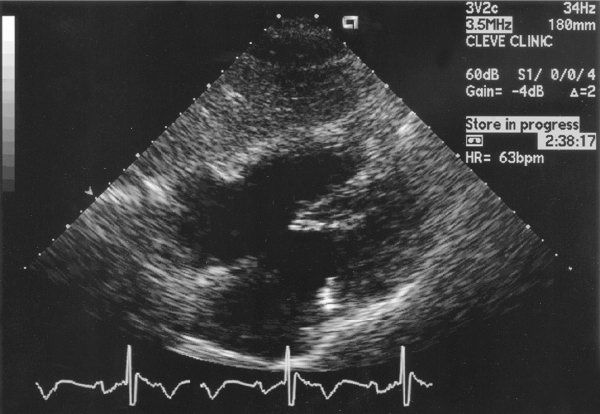
Figure 9.10
Intracardiac Shunts
42.Which of the following are associated with patent foramen ovale (PFO)?
a.Migraine
b.Platypnea-orthodeoxia
c.Decompression sickness
d.Paradoxical embolism & stroke
e.All of the above
43.A 25-year-old man is referred to you for an abnormal heart sound. The patient is asymptomatic and very active. BP is 130/50 mmHg. He has a continuous murmur at the left upper sternal border. A TTE reveals a small PDA with mildly dilated left atrium (LA) and mildly dilated LV but normal RV size and normal pulmonary pressures. How would the patient be best managed?
a.Ligation or percutaneous closure of the PDA
b.Repeat TTE in 1 year
c.Stress echocardiography to determine LV enlargement or dysfunction postexercise
d.Pulmonary vasodilator
e.TEE
44.Which of the following is most commonly associated with a sinus venosus ASD?
a.Coarctation of the aorta
b.Bicuspid aortic valve
c.Anomalous right pulmonary venous connection
d.Inlet VSD
e.Persistent left SVC
45.The best echocardiographic scan plane for demonstrating a secundum ASD is
a.apical four-chamber view.
b.parasternal long-axis view.
c.parasternal short-axis view.
d.subcostal four-chamber view.
e.suprasternal long-axis view.
46.Review the image taken at the time of percutaneous closure of an intracardiac shunt in a 25-year-old patient (Fig. 9.12). Which of the following defects was closed in this patient?
a.Primum ASD
b.Secundum ASD
c.Sinus venosus ASD
d.Unroofed coronary sinus
e.Atrioventricular septal defect (AVSD)

Figure 9.12
47.Secundum ASDs may be associated with
a.pulmonary hypertension.
b.mitral valve prolapse.
c.partial anomalous pulmonary venous connection.
d.pulmonic stenosis.
e.all of the above.
48.Which type of VSD is demonstrated in Figure 9.13?
a.Type 1/supracristal
b.Type 2/perimembranous
c.Type 3/inlet
d.Type 4/muscular
49.Percutaneous VSD closure is approved by the U.S. Food and Drug Administration for which type of VSD?
a.Type 1/supracristal
b.Type 2/perimembranous
c.Type 3/inlet
d.Type 4/muscular
e.None: Surgery is the only approved treatment for VSD closure
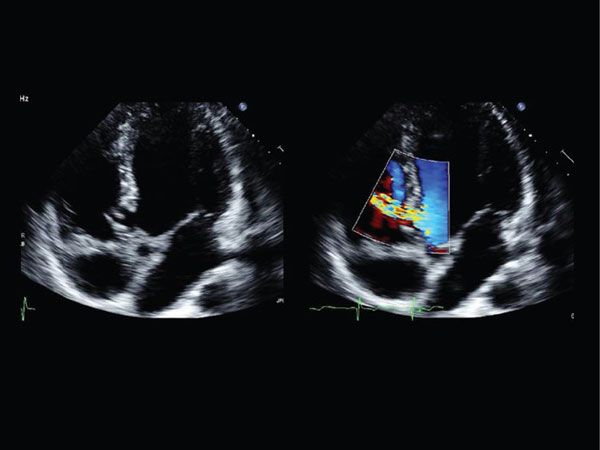
Figure 9.13
Left-Sided Lesions
50.What is the most common coexisting congenital anomaly in patients with coarctation of the aorta?
a.Cleft mitral valve
b.Bicuspid aortic valve
c.Ebstein anomaly
d.VSD
e.PDA
51.A 20-year-old man is referred for further evaluation of hypertension. He has remained hypertensive despite a 12-week trial of β-blocker treatment. Examination reveals a right upper extremity BP of 150/100 mmHg and a right lower extremity BP of 130/90 mmHg. HR is 88 bpm. There is brachial– femoral pulse delay. The rest of the physical and neurologic examinations are within normal limits. A TTE confirmed a diagnosis of coarctation of the aorta, with a maximum gradient of 30 mmHg. He is referred for cardiac catheterization. Intervention for coarctation is recommended when the coarctation gradient is greater than which of the following?
a.10 mmHg
b.20 mmHg
c.40 mmHg
d.60 mmHg
e.None of the above; indications for intervention in coarctation are determined by symptoms and not the coarctation gradient
52.Which of the following is the most common coronary artery anomaly?
a.Bland-Garland-White syndrome (left main coronary arising from the PA)
b.Coronary arteriovenous fistula
c.Left circumflex artery arising from the right coronary artery
d.Left coronary artery arising from the right sinus of Valsalva
e.Coronary cameral fistula
53.Which of the following statements about coronary arteriovenous fistula is true?
a.The left coronary artery is most commonly involved.
b.The fistula most commonly empties into the LV.
c.Despite the success of surgical closure, the prognosis is still poor.
d.Spontaneous closure rarely occurs.
e.A large right-to-left shunt may cause congestive heart failure (CHF).
54.Which of the following differentiates valvular aortic stenosis from subvalvular aortic stenosis?
a.Male preponderance
b.Surgical risk of repair
c.Dilatation of the ascending aorta
d.Aortic regurgitation
e.Valvular calcification
55.Echocardiography in a 20-year-old asymptomatic man reveals a subaortic membrane with a peak gradient of 20 mmHg. The aortic valve remains mobile, but there is associated mild to moderate aortic valve insufficiency. LV size is normal ejection fraction is 60%. What should you advise this patient?
a.There is no indication for intervention at this time.
b.Surgical resection of the membrane and debridement of the aortic valve to reduce aortic regurgitation is indicated.
c.Transluminal balloon dilatation is the best treatment option in this case.
d.AVR and membrane resection is indicated.
56.The peak age range for surgical intervention for patients with a bicuspid aortic valve is
a.10 to 20 years.
b.20 to 40 years.
c.40 to 60 years.
d.60 to 80 years.
Right-Sided Lesions
57.A 45-year-old man with known Ebstein anomaly seeks your advice with regard to optimal management. He is asymptomatic and has an active lifestyle without any limitations. His physical examination is remarkable for the absence of cyanosis. He has a loud holosystolic murmur at the left lower sternal border that is accentuated with respiration. He has no organomegaly or peripheral edema. His TTE reveals moderately severe 3+ TR with an RV systolic pressure of 35 mmHg and normal LV and RV systolic function. There is no evidence of interatrial communication. Which of the following should you recommend?
a.Furosemide and digoxin
b.Tricuspid valve repair
c.Tricuspid valve replacement
d.Dual-chamber pacemaker
e.Regular follow-up with repeat TTE in 6 months
58.The most common problem in adults with surgically repaired TOF is
a.ventricular tachycardia.
b.pulmonary hypertension.
c.pulmonary regurgitation.
d.cyanosis.
e.residual VSD.
59.A 34-year-old gentleman reports a history of TOF,
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


