Statins are the primary agents used to decrease low-density lipoprotein cholesterol. Although adherence to statins improves the clinical outcomes, the affect of statin adherence on healthcare costs has not been well studied. To examine the relation among statin adherence, subsequent hospitalizations, and healthcare costs, we conducted a retrospective cohort study of 381,422 patients, aged 18 to 61 years, using an integrated pharmacy and medical claims database. We measured adherence using the medication possession ratio (MPR) for 12 months and the healthcare costs and cardiovascular disease-related hospitalizations during the subsequent 18 months. Of those studied, 258,013 (67.6%) were adherent (MPR ≥80%), 65,795 (17.3%) had an MPR of 60% to 79%, and 57,614 (15.1%) had an MPR of <60%. The adjusted all-cause total healthcare costs were lowest in the adherent group at $10,198 ± $39.4 (mean ± SE) versus $10,609 ± $77.7 (p <0.001) for an MPR of 60% to 79%, and $11,102 ± $84.3 (p <0.001) for an MPR of <60%. The adherent group had greater statin costs at $838 ± $1.0 versus $664 ± $2.0 (p <0.001) and $488 ± $2.2 (p <0.001). When evaluated by 5 levels of MPR, 0% to 59% and increments of 10% >60%, the adjusted total healthcare costs were lowest for the MPR 90% to 100% group and significantly greater statistically (p <0.001) for each lower level of adherence. Compared to the statin-adherent patients, cardiovascular disease-related hospitalizations were more likely for the patients with an MPR of 60% to 79% (odds ratio 1.12, 95% confidence interval 1.08 to 1.16) and an MPR of 0% to 59% (odds ratio 1.26, 95% confidence interval 1.21 to 1.31). In conclusion, statin adherence is associated with reductions in subsequent total healthcare costs and cardiovascular disease-related hospitalizations.
Although adherence to statins has been shown to affect clinical outcomes, limited data are available evaluating the healthcare costs associated with better adherence. The objective of the present study was to evaluate adherence to statins for 12 months to determine the affect on healthcare costs and cardiovascular-related hospitalizations in the subsequent 18 months.
Methods
The source of data was the Medco National Integrated database, which contains 30 months of medical and pharmacy claims data for approximately 13 million patients enrolled in >450 different health plans, including fee-for-service, preferred provider, and managed care plans sponsored by insurance companies, employers, and government organizations. The medical claims contain all inpatient, outpatient, nursing home, laboratory, and diagnostic testing claims the health plan has received. The laboratory tests and medical care paid out of pocket or through Medicare are not included in the database.
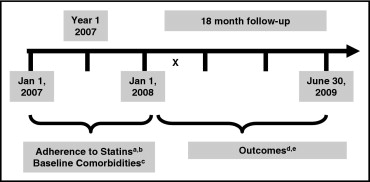
The study consisted of a cohort of all patients aged 18 to 61 years as of January 1, 2007, with at least one pharmacy claim for a statin medication from January 1, 2008 to June 30, 2008 and a second claim within 12 months before the last claim seen before June 30, 2008. The statins included in the present analysis are listed in Figure 1 . We excluded patients with claims for malignant neoplasms ( International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] codes 140* to 172* and 174* to 209*), except for those with nonmelanoma skin cancer, or human immunodeficiency virus infection (ICD-9-CM codes 042 and V08), because these diseases can be associated with overwhelming pharmacy and medical costs, independent of the adherence to statins. In addition, we limited our analysis to patients with continuous eligibility for pharmacy and medical benefits from January 1, 2007 through June 30, 2009. The baseline year was January 1, 2007 to December 31, 2007, and the 18-month follow-up was January 1, 2008 to June 30, 2009 ( Figure 1 ). The selection criteria were used to create a de-identified data set that was further analyzed for the present study.
The adherence to statins was estimated by calculating the medication possession ratio (MPR) or the ratio of total days of medication supplied to the total days within a set period. The MPR is the accepted standard for the evaluation of adherence using retrospective data, because it is easy to calculate and performs as well as other claims-based estimates. MPR was calculated according to the total number of days between the dates of the last filling of a statin prescription in the first 6 months of 2008 and the first filling of a statin prescription in the 365 days before the last filling. If the patient had received one or more statins during the 365-day adherence measurement period, the days’ supply for all statins were included in the calculation. The MPR was capped at 100%, because it was unlikely that patients would have used the statins at greater than the prescribed frequency.
For the primary evaluation, we used the MPR to classify the patients into 3 adherence categories: adherent (MPR ≥80%), moderate adherence (MPR 60% to 79%), and low adherence (MPR <0% to 59%). Previous data have recommended using the MPR as a dichotomous variable, with an MPR of 80% considered adherent. Although this proportion is somewhat arbitrary, it has been accepted as the cutoff for adherence in most studies of adherence. We performed secondary analyses using 5 levels of adherence: MPR of 0% to 59%, 60% to 69%, 70% to 79%, 80% to 89%, and 90% to 100%.
The number of all medications “on hand” was determined as of the last day of the baseline year. We evaluated the variables likely to be associated with adherence during the baseline period, including the proportion of statin prescriptions filled with generic statins; the proportion of the total statin days’ supply filled by mail; and the patient co-payment for statins per month (i.e., the total amount patients paid for their statins, including the co-payment, deductible, and co-insurance per month).
For each patient, we used the medical claims to determine the presence of one or more hospitalizations in the baseline year and follow-up period. We also used medical claims to identify specific co-morbidities using the ICD-9-CM diagnosis codes shown in Figure 1 . The primary outcome was the identification of the total all-cause healthcare costs in the subsequent 18-month follow-up period, January 1, 2008 to June 30, 2009, among the low adherence, moderate adherence, and adherent groups. The total all-cause healthcare costs were calculated as the sum of all pharmacy and medical costs (including outpatient services, emergency department services, and hospitalizations) paid by the plan sponsor during the 18-month follow-up period and excluded patient co-payments and deductibles. Secondary analyses were conducted by further analyzing the cost of statins, the cost of medications other than statins, all-cause medical costs, and cardiovascular disease (CVD)-related medical costs. We evaluated the association between the adherence levels and the risk of one or more CVD-related hospitalizations during the 18-month follow-up period using ICD-9-CM codes in Figure 1 .
We compared the baseline demographic factors, co-morbidities, and medication factors between the adherent and nonadherent patients using the chi-square test for binary variables and the t test for continuous variables. Regression analyses were performed to assess the relation between the outcome variables and covariates. Logistic regression analysis was used to reveal the determinants of adherence to statins (defined as an MPR of ≥80%). The predictors included age, gender, co-morbidities, chronic disease score, out-of-pocket costs for medication, and the use of mail-order pharmacy. Logistic regression analysis was also performed for 2 additional models to evaluate the association among 3 levels of adherence and adherence as a continuous variable with clinical outcomes of CVD-related hospitalization, after adjusting for important baseline differences. To determine the average costs in the 18-month follow-up period for each level of adherence, we used generalized linear models and adjusted for baseline differences in age, gender, year 1 co-morbidities, the year 1 total number of medications, and the year 1 total healthcare costs. The least square mean of the costs were generated and compared among the 3 adherence groups. SAS, version 9.1 (SAS Institute, Cary, North Carolina), was used for all the statistical analyses, and 2-sided p values of <0.05 were considered statistically significant.
Results
Our analysis identified 381,422 patients who met the inclusion criteria. The patient demographics are listed in Table 1 . The mean level of adherence in year 1 was 43.1% in the MPR <60% group, 71.3% in the 60% to 79% adherence group, and 94.5% in the MPR ≥80% adherent group.
| Variable | All Patients | Adherence Level | ||||
|---|---|---|---|---|---|---|
| Low (MPR 0–59%) | Moderate (MPR 60–79%) | Adherent (MPR 80–100%) | p Value | |||
| Adherent vs Moderate | Adherent vs Low | |||||
| Patients | 381,422 (100%) | 57,614 (15.1%) | 65,795 (17.3%) | 258,013 (67.6%) | <0.0001 | <0.0001 |
| Age (years) | 53.0 ± 6.71 | 51.6 ± 7.31 | 52.0 ± 7.02 | 53.6 ± 6.41 | <0.0001 | <0.0001 |
| 18–44 | 44,886 (11.8%) | 9,772 (17.0%) | 9,882 (15.0%) | 25,232 (9.8%) | <0.0001 | <0.0001 |
| 45–54 | 145,002 (38.0%) | 23,713 (41.2%) | 27,174 (41.3%) | 94,115 (36.5%) | <0.0001 | <0.0001 |
| 55–64 | 191,534 (50.2%) | 24,129 (41.9%) | 28,739 (43.7%) | 138,666 (53.7%) | <0.0001 | <0.0001 |
| Women | 158,044 (41.4%) | 25,836 (44.8%) | 27,071 (41.1%) | 105,137 (40.8%) | 0.065 | <0.0001 |
| Mean adherence (MPR) | 82.7 ± 20.2% | 43.1 ± 12.9% | 71.3 ± 5.9% | 94.5 ± 6.1% | <0.0001 | <0.0001 |
| Co-morbidities | ||||||
| Coronary artery disease | 57,811 (15.2%) | 7,725 (13.4%) | 9,111 (13.8%) | 40,975 (15.9%) | <0.0001 | <0.0001 |
| Diabetes mellitus | 96,950 (25.4%) | 15,253 (26.5%) | 16,375 (24.9%) | 65,322 (25.3%) | 0.024 | <0.0001 |
| Hypertension | 198,661 (52.1%) | 28,587 (49.6%) | 32,587 (49.5%) | 137,487 (53.3%) | <0.0001 | <0.0001 |
| Stroke | 12,893 (3.4%) | 1,848 (3.2%) | 2,093 (3.2%) | 8,952 (3.5%) | <0.0001 | 0.002 |
| Peripheral artery disease | 4,574 (1.2%) | 693 (1.2%) | 780 (1.2%) | 3,101 (1.2%) | 0.730 | 0.985 |
| Heart failure | 6,821 (1.8%) | 1,039 (1.8%) | 1,163 (1.8%) | 4,619 (1.8%) | 0.696 | 0.830 |
| Depression | 32,623 (8.6%) | 5,113 (8.9%) | 5,918 (9.0%) | 21,592 (8.4%) | <0.0001 | <0.0001 |
| Mean total medications | 3.4 ± 2.7 | 2.2 ± 2.3 | 2.9 ± 2.5 | 3.7 ± 2.7 | <0.0001 | <0.0001 |
| Mean generic statin use (%) | 35.6 ± 46.64% | 33.0 ± 45.52% | 34.5 ± 45.97% | 36.5 ± 47.03% | <0.0001 | <0.0001 |
| Mean statins by mail (%) | 48.9 ± 48.00% | 27.3 ± 43.14% | 40.0 ± 46.81% | 56.0 ± 47.49% | <0.0001 | <0.0001 |
| Mean statin co-pay ($/mo) | $16.20 ± 14.58 | $19.32 ± 24.52 | $17.33 ± 12.55 | $15.22 ± 11.68 | <0.0001 | <0.0001 |
| ≥1 Hospitalizations | 28,875 (7.6%) | 4,495 (7.8%) | 4,976 (7.6%) | 19,404 (7.5%) | 0.713 | 0.021 |
| ≥1 Emergency department visits | 54,304 (14.2%) | 9,508 (16.5%) | 10,023 (15.2%) | 34,773 (13.5%) | <0.0001 | <0.0001 |
| Year 1 total healthcare costs | $6,523 ± 15,499 | $5,630 ± 13,548 | $6,314 ± 18,999 | $6,776 ± 14,893 | <0.0001 | <0.0001 |
Overall, the most common co-morbidities were hypertension, coronary artery disease, and diabetes mellitus. Also, 8.6% of the patients had a history of depression. The adherent group was older, more likely to be men, and had a greater proportion of patients with an ICD-9-CM claims diagnosis of coronary artery disease, hypertension, or stroke. In addition, the adherent group had significantly more generic statin use, a lower statin co-payment, and greater mail order statin use. In the fully adjusted multivariate logistic regression analysis that modeled the predictors of adherence, the patients who received >80% of their statins by mail (odds ratio [OR] 2.16, 95% confidence interval [CI] 2.13 to 2.19) were older (OR 1.02 for each year, 95% CI 1.02 to 1.03) or had more total active medications available at the end of the baseline year (OR 1.27 for each additional medication, 95% CI 1.27 to 1.28) and were more likely to be adherent. In contrast, patients with an ICD-9-CM for depression (OR 0.82, 95% CI 0.80 to 0.84) or who had paid >$10/mo in co-payments for their statins were less likely to be adherent (OR 0.75, 95% CI 0.73 to 0.76).
The adjusted all-cause total healthcare costs and medical costs were lowest and the statin costs were greatest in the adherent group ( Table 2 ). The costs associated with the 5 levels of MPR from 0% to 59% and increments of 10% >60% are shown in Figure 2 . In an additional analysis that evaluated the association between MPR as a continuous variable and healthcare costs, we found similar statistically significant associations between a greater MPR and lower medical and total healthcare costs. Adherent patients had adjusted CVD-related medical costs of $2,395 ± 20.5 SE compared to patients with moderate ($2,583 ± $40.4) and low ($2,689 ± $43.9) adherence (p <0.001). The CVD-related total healthcare costs were not significantly different statistically among the groups.



