Adenosquamous Carcinoma
Marie-Christine Aubry, M.D.
Allen P. Burke, M.D.
General
Adenosquamous carcinoma is composed of an adenocarcinoma and squamous cell carcinoma component comprising at least 10% of the whole tumor.1,2,3 Various hypotheses for the pathogenesis of adenosquamous carcinomas include primarily adenocarcinomas with squamous differentiation, collision tumors, a variant of high-grade mucoepidermoid carcinoma, or tumors of pluripotential undifferentiated cell origin.4
Clinical
Radiologic Findings
Gross Findings
Microscopic Findings
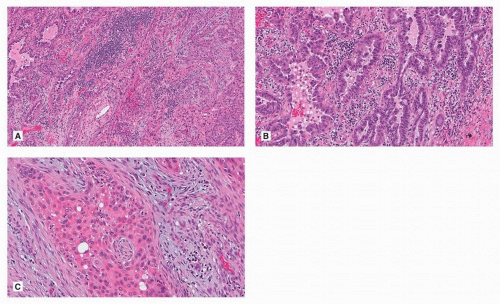
Adenosquamous cell carcinoma morphologically shows two distinct cell population. The adenocarcinoma is acinar, papillary, or lepidic or a combination of these, in ˜75% of tumors (Fig. 83.1). In about 25% of cases, the adenocarcinoma is solid comprised of only large cells or cribriform. If entirely solid, it is confirmed as adenocarcinoma by immunohistochemical staining for TTF-1.10 By definition, the squamous component shows keratinization or intercellular bridges.
Adenosquamous carcinomas are more likely than other non-small cell carcinomas to have lymphatic, blood vessel, and visceral pleural invasion (11%, 20%, and 30%, respectively).9
Immunohistochemistry
Immunohistochemistry is not necessary if the two population of cells, adenocarcinoma and squamous cell carcinoma, are morphologically recognizable by regular H&E. But in cases where the adenocarcinoma component is solid and the squamous cell carcinoma nonkeratinizing and higher grade, performing TTF-1 and p40 assists with the diagnosis. As with morphology, the immunoprofile reveals two distinct population of cells, one that is TTF-1 positive and a separate that is p40 positive. Rarely, TTF-1-positive cells may be seen in squamous cell carcinoma and p40 in adenocarcinoma. This does not constitute an adenosquamous cell carcinoma (Fig. 83.2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree