Adenoid Cystic Carcinoma
Presentation
A 62-year-old woman presented to her primary care doctor because of a persistent cough for the past 4 weeks. The primary care physician noted some wheezing and treated her for a presumptive diagnosis of asthma. She was referred to a thoracic surgeon after she expectorated blood-tinged mucus.
The patient denies fever, occupational exposures, or any travel history. Her past medical history includes diabetes. She is a former smoker and has a 20-packper-year smoking history.
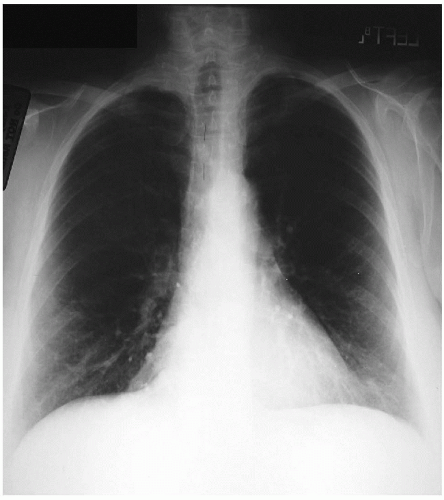
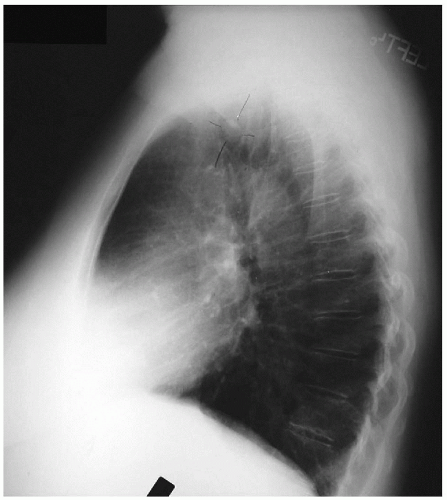
The physical examination reveals a moderately obese woman who is in no respiratory distress. There is no cervical adenopathy. Her cardiac tones are normal. Inspiratory wheezing is present on auscultation of her chest. She presents with the following chest x-rays.
▪ Chest X-rays
Chest X-ray Report
This study demonstrates a 1.5-cm rounded density within the trachea. The heart and great vessels are normal. The lung fields are clear.
Discussion
Adult-onset asthma is unusual. A tracheal tumor should be considered in the differential diagnosis of patients with a persistent cough and wheezing, especially with associated hemoptysis.
Primary tracheal tumors are rare; they may be benign or malignant. One third of tracheal tumors are squamous cell carcinoma; one third are adenoid cystic carcinoma; and one third have a variety of benign and malignant causes. Squamous cell carcinoma tends to occur posteriorly in the distal one third of the trachea. Adenoid cystic carcinoma, formerly known as cylindroma, is more common in the upper one third of the trachea. Other malignant tumors of the trachea include carcinoid tumors, which include typical and atypical histologic types, adenocarcinoma, and small cell carcinoma.
Benign tumors tend to be round and smooth. Calcification within the tumor usually indicates a benign process. This is seen in hamartomas and chondromas. The exception is chondrosarcoma, which is malignant and may have calcifications. Other benign tumors of the trachea include papillomas, fibromas, and hemangiomas. Malignant tumors are irregular and may be ulcerated. Hoarseness usually signifies malignancy with involvement of the recurrent laryngeal nerve. Secondary malignant tracheal tumors include tumor extension from the larynx or thyroid, lung cancer, esophageal cancer, and metastatic disease from a distant primary cancer.
Cough is a common symptom associated with tracheal tumors. Wheezing and stridor are caused when the airway narrowing becomes more profound. This wheeze is more prominent during inspiration and is different from that of asthma, which occurs in expiration. Dyspnea and shortness of breath are common presenting features and occur when the tracheal cross-sectional area is reduced to one-third its original size. Hemoptysis occurs in 25% of patients and is most commonly seen with squamous cell carcinoma. Benign tumors are usually not associated with hemoptysis.
Many patients with tracheal tumors have a delayed diagnosis because of seemingly normal appearance of their chest x-ray. Careful inspection of the tracheal air column on plain chest x-rays is essential and may demonstrate the presence of a tracheal neoplasm, as it does in this patient. Tomograms and oblique and lateral views of the trachea using soft tissue technique visualize most tumors. Maneuvers such as swallowing and neck hyperextension may be used to demonstrate disease located in the upper trachea. These imaging techniques have largely been replaced by thin-cut computed tomography (CT) scans and magnetic resonance imaging (MRI) studies.
CT scans can be used to generate high-resolution images of the trachea, especially if thin (3-mm) cuts are obtained. The presence and degree of obstruction and invasion of the trachea, as well as lymph node involvement, can be assessed using high-resolution CT scanning. MRI, although not absolutely necessary, may provide enhanced images that aid in preoperative determination of the degree of invasion into surrounding tissues and blood vessels. The coronal and sagittal views are useful in determining the length of the tracheal neoplasm. Barium esophagogram may demonstrate esophageal compression or invasion and should be obtained in cases in which dysphagia is also present. Pulmonary function tests show the classic obstructive pattern, with a decreased forced expiratory volume in 1 section (FEV1) and peak flow rate. The expiratory flow-volume loop is flattened.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree