performed with the catheter in this position. If the case proceeds to carotid stent placement, the elbow or secondary curve of the catheter must be advanced into the artery at its origin to obtain exchange guidewire access to the common carotid artery. Carotid artery catheterization is discussed in more detail below.
Table 29-1 Skills Required for Carotid Angioplasty and Stenting | ||||||
|---|---|---|---|---|---|---|
|
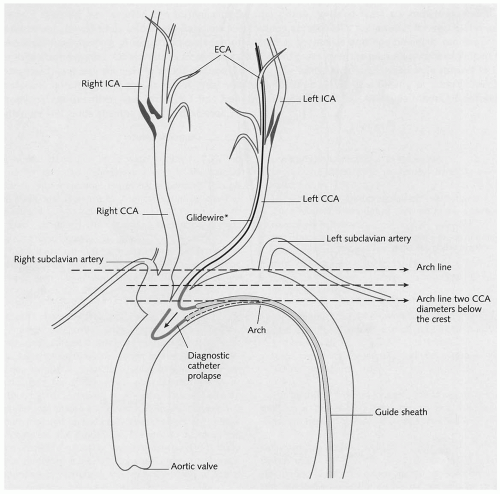
not become inadvertently dislodged into the carotid bulb with breathing or arterial pulsation. The external carotid artery is roadmapped, and the best branch for anchoring the carotid sheath is chosen. The guidewire is advanced into the distal external carotid artery branch and is followed by the catheter. The Glidewire is subsequently removed. The selective cerebral catheter must be back bled to avoid introducing air into the system. This often requires withdrawing the catheter slightly, because its tip usually enters a small, distal branch. The exchange guidewire is then placed in the external carotid artery. Commonly used exchange guidewires are the Amplatz super-stiff (Cook, Inc., Bloomington, IN) or extra-stiff (Boston Scientific), the Supracore (Guidant, Menlo Park, CA), the Microvena Nitinol (Microvena Corp., White Bear Lake, MN), or a Stiff Glidewire (Boston Scientific). A braided, selective catheter is useful when advancing the stiff exchange guidewire into the external carotid artery, because it is less likely to be pulled out. After the exchange guidewire has been placed, the selective catheter is removed and the long, carotid guiding sheath is inserted. The guidewire is surveyed with fluoroscopy to look for any redundant segments; these should be removed before sheath passage. The 6 Fr sheath is commonly used with popular ones, including the Shuttle Sheath (Cook), Destination (Boston Scientific), and Vista Brite Tip (Cordis Corp., Miami Lakes, FL). The sheath is advanced over the exchange guidewire with steady forward pressure. The field of view should include the guidewire tip and the course of the guidewire from the arch into the common carotid artery to make certain that the guidewire is not migrating caudally. When the sheath tip reaches the last major turn from the arch into the common carotid artery, the angle of approach can be made less acute by having the patient take a deep breath.
and the lower profile. The main disadvantage of the monorail system is that it must be delivered directly into the side branch through a long sheath (rather than over a large-caliber guidewire). There is a learning curve associated with its use, but experienced vascular specialists consider it easier and faster than the standard coaxial system.
Table 29-2 Pitfalls Associated with Remote Access and Working Through a Long Sheath | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
The refinement of its accuracy to determine the degree of stenosis
The benefits of the arteriogram, in terms of reducing the complication rates of the open repair, do not outweigh its small risk
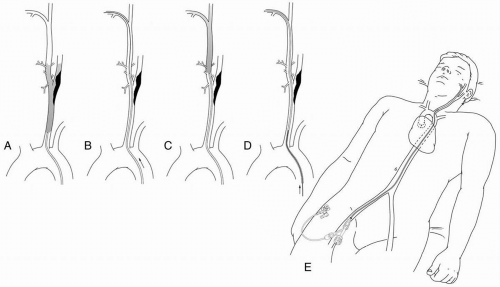
sheath is directed toward the surgeon, and pressure is maintained at the arteriotomy with the nondominant hand until the sheath enters the artery.
Table 29-3 Comparison of Coaxial and Monorail Systems | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Table 29-4 Current Indications for Carotid Arteriography for Extracranial Carotid Artery Occlusive Disease | ||||
|---|---|---|---|---|
|