Acutely Thrombosed Bypass Graft (Including Lytics)
AMY B. REED
Presentation
A 57-year-old man arrives in the emergency department complaining of a 3-day history of a cool, painful left foot. He had previously undergone an aortobifemoral bypass graft at an outside institution. He is now 1 year out from a left femoral to posterior tibial artery bypass graft with greater saphenous vein, which you performed for rest pain after his prosthetic femoral above-knee popliteal artery bypass graft had occluded. On examination, the femoral pulses are palpable bilaterally. The left foot is cool and slightly mottled with a monophasic Doppler signal over the posterior tibial artery. The bypass graft is nonpalpable. His motorsensory examination is normal, except for slight numbness over the plantar arch.
Differential Diagnosis
The differential diagnosis for acute lower extremity ischemia typically includes arterial thrombosis secondary to underlying atherosclerotic arterial occlusive disease, atheromatous embolization from a more proximal unstable plaque, or thromboembolism from an aortic aneurysm or cardiac source. Early deep vein thrombosis can present in a similar manner; however, the leg will typically be swollen. Other less common causes of acute limb ischemia, such as thrombosed popliteal artery aneurysm, popliteal entrapment, and severe vasospasm, must also be kept in mind. In this patient with a previous history of peripheral bypass surgery, graft thrombosis must be considered the primary diagnosis.
Recommendation
After systemic heparinization, the initial diagnostic test in this patient is an aortogram with left lower extremity arteriogram. Acute limb ischemia is stratified into four categories based on severity and limb threat: class I—limb viable; class IIa—limb marginally threatened; class IIb—limb immediately threatened; and class III—irreversible limb changes. Patients with class I or IIa ischemia often have time for angiography and possible thrombolytic therapy in a semielective fashion, whereas patients with class IIb and early III typically require immediate revascularization. This patient has class IIa ischemia and would be best served by arteriography with possible thrombolysis of the suspected graft thrombosis.
Arteriography Report
Aortogram with left lower extremity runoff reveals a patent aortobifemoral bypass graft with occlusion of the superficial femoral, popliteal, and anterior tibial arteries. The stump of the bypass graft at the proximal anastomosis is visualized; however, the remainder of the graft is occluded. The posterior tibial artery is reconstituted in the proximal third of the calf.
Discussion
Catheter-directed thrombolysis for class I or IIa limb ischemia has several potential advantages, including more gentle clot lysis, the ability to clean out the involved segment as well as the distal vessels, and potentially revealing the underlying stenotic lesion. The decision to proceed with angiography and possible thrombolysis is dictated by the severity of the ischemia and perceived limb threat.
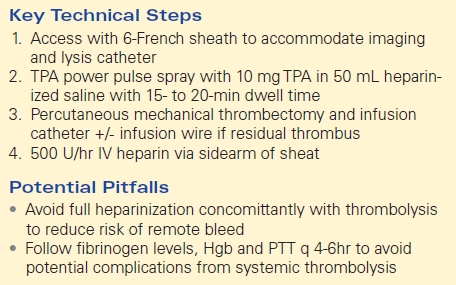
Approach
A Teflon-coated 0.035” wire is used to select the stump of the proximal anastomosis and is able to be manipulated into the mid-portion of the occluded bypass graft. Percutaneous mechanical thrombectomy with a pulse spray of tissue plasminogen activator (TPA) 10 mg in 50 mL saline is laced throughout the extent of the thrombus. After 15 to 20 minutes of dwell time, percutaneous mechanical thrombectomy is performed. Repeat arteriography will typically show resolution of the thrombus and reveal the underlying culprit stenosis. If a significant amount of thrombus persists despite thrombectomy, an infusion catheter running TPA 1 mg/h along with systemic unfractionated heparin at 500 U/h may be run overnight. A repeat arteriogram is performed (Table 1 and Figure 1).
TABLE 1. Key Steps and Potential Pitfalls of Thrombolysis