Acute Pulmonary Consolidation
Jonathan H. Chung, MD
DIFFERENTIAL DIAGNOSIS
Common
Pneumonia
Cardiogenic Pulmonary Edema
Atelectasis
Aspiration
Pulmonary Contusion
Pulmonary Hemorrhage
Less Common
Hypersensitivity Pneumonitis (Acute)
Diffuse Alveolar Damage
Pulmonary Infarct
Rare but Important
Acute Eosinophilic Pneumonia
“Crack Lung”
ESSENTIAL INFORMATION
Helpful Clues for Common Diagnoses
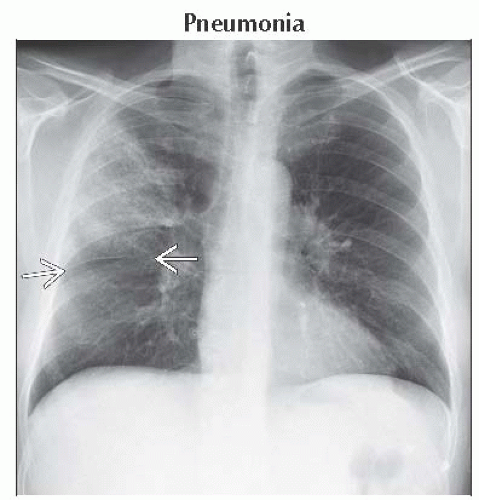
Pneumonia
Airspace opacities: Ground-glass to dense consolidation
Reactive lymphadenopathy; very large lymph nodes unusual
Parapneumonic pleural effusion or empyema
Correlation with sputum, WBC count, and clinical presentation paramount
Cardiogenic Pulmonary Edema
Due to imbalances in Starling forces: Usually due to increased pulmonary venous pressure
Left-sided heart failure (myocardial infarct or ischemic cardiomyopathy)
Fluid overload or renal failure
Mitral valve disease
Interlobular septal thickening: Kerley-B and Kerley-A lines on chest radiograph
Diffuse, hazy airspace opacities
Characteristically central-predominant due to higher concentration of lymphatics in peripheral aspect of lungs
Cardiomegaly frequently noted
Signs of coronary artery disease (coronary artery calcification, CABG, coronary artery stents, subendocardial fatty metaplasia)
Atelectasis
Subsegmental
Discoid or linear opacity most often in mid and lower lungs
Hypoventilation or decreased diaphragmatic excursion (splinting, neuromuscular abnormality, subdiaphragmatic mass effect)
Small airways disease (secretions leading to resorptive atelectasis, asthma, viral bronchiolitis)
Decreased surfactant production (pulmonary embolism)
Compression (mass effect from adjacent pathology)
Lobar
Lobar volume loss: Displacement of pulmonary fissures, ipsilateral shift of mediastinum and hilum toward affected lobe, superior shift of diaphragm
Increased opacity of affected lobe
Combined right middle and lower lobe atelectasis from bronchus intermedius obstruction; mimics pleural effusion
In acute setting, most often due to obstruction of bronchus due to mucous plugging or foreign body
Aspiration
Consolidation in gravity-dependent portions of lungs
Predisposed patients (e.g., those with alcoholism, epilepsy, hiatal hernia, esophageal dysmotility or obstruction, neuromuscular disorders)
Supine: Superior segments of lower lobes and posterior segments of upper lobes
Upright: Basilar segments of lower lobes
Centrilobular or tree in bud opacities common on CT
Can progress to necrotizing pneumonia or pulmonary abscess without treatment
Pulmonary Contusion
Acute blunt trauma; appears at time of injury and resolves in 3-5 days
Peripheral, under point of blunt kinetic energy absorption
Often lateral portions of lung away from overlying musculature
Overlying rib fractures; but can occur without rib fractures in children and young adults
Pulmonary Hemorrhage
Widespread
Vasculitis, anticoagulation, idiopathic pulmonary hemosiderosis
Focal
Mass, aspiration, bronchiectasis, trauma
Ground-glass opacities > consolidation; may be diffuse, patchy, lobular, or centrilobular
Tendency to spare peripheral, apical, and costophrenic aspects of lungs
Increased interlobular and intralobular septal thickening over 1-2 days
Rapid resolution in days, though not as rapid as in cardiogenic pulmonary edema or bland aspiration
In recurrent hemorrhage, may result in lung fibrosis
Helpful Clues for Less Common Diagnoses
Hypersensitivity Pneumonitis (Acute)
Allergic reaction to airborne organic particles
Diffuse or centrilobular ground-glass opacities; lobular air-trapping
Diffuse Alveolar Damage
Noncardiogenic pulmonary edema
Clinical correlate is acute respiratory distress syndrome
Heterogeneous, diffuse ground-glass opacities and consolidation
Often with anterior-posterior and superior-inferior gradient
Large pleural effusions and severe interlobular septal thickening uncommon
Varicoid bronchiectasis, reticular opacities, and honeycombing common 2-3 weeks after onset of respiratory distress
Pulmonary Infarct
Most often from pulmonary arterial embolism
Often in setting of superimposed cardiac dysfunction (cardiomyopathy, congestive heart failure)
Lower lung predominant, peripheral/subpleural, wedge-shaped consolidation: Hampton hump sign
Resolves over months; retains its original shape rather than patchy resolution as in pneumonia
Helpful Clues for Rare Diagnoses
Acute Eosinophilic Pneumonia
Probable hypersensitivity reaction to inhaled agents; possible association with smoking
Imaging mimics pulmonary edema
Ground-glass opacities > consolidation
Interlobular septal thickening
Pleural effusions
Acute high fever, profound dyspnea, myalgia, pleuritic chest pain
Responds rapidly to steroids
“Crack Lung”
“Crack” = smoked form of cocaine
Hypersensitivity reaction, pulmonary hemorrhage, pulmonary edema (cardiogenic and noncardiogenic)
Noncardiogenic pulmonary edema may be peripheral and bilateral as opposed to cardiogenic edema
Pneumomediastinum or pneumothorax
Image Gallery
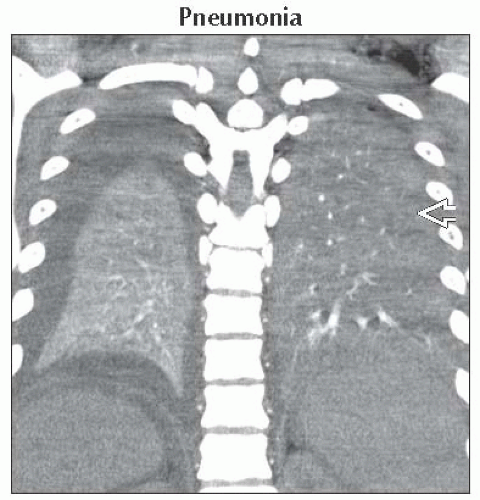 Coronal CECT shows consolidation of both lower lobes. The lower attenuation of the left lower lobe
 suggests superimposed pneumonia or aspiration, while the denser right lower lobe suggests atelectasis. suggests superimposed pneumonia or aspiration, while the denser right lower lobe suggests atelectasis.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|