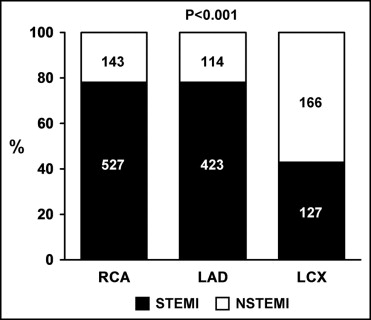
Acute occlusion of the left circumflex (LC) artery can be difficult to diagnose. The aim of the present study was to assess the incidence of LC occlusion in patients with acute myocardial infarction (AMI) requiring percutaneous coronary intervention (PCI), the frequency of ST-segment versus non–ST-segment elevation presentation among them, and to correlate the electrocardiographic findings with the outcomes. The clinical characteristics and outcomes of consecutive patients from November 2001 through December 2007 with AMI within 7 days before PCI of a single acutely occluded culprit vessel were included in the present analysis. Of the 1,500 patients, the culprit lesion was located in the right coronary artery, left anterior descending artery, or LC artery in 44.7%, 35.8%, and 19.5% of patients, respectively. Of the 1,500 patients, 72% presented with ST-segment elevation AMI, but only 43% were patients with a LC lesion (n = 127). PCI was significantly less likely (80%, 83%, and 70% for right coronary, left anterior descending, and LC artery, respectively; p <0.001) to be performed within 24 hours for LC occlusions than for occlusions in the other territories. Among those with a non–ST-segment elevation AMI, the highest post-PCI troponin levels were in patients with a LC artery occlusion (median 1.4, 1.3, and 2.5 ng/ml; p <0.001). No significant difference was found in the in-hospital mortality (4.4%, 7.4%, and 6.5%; p = 0.66) or major adverse cardiovascular event (9.2%, 13.9%, and 11.6%; p = 0.53) rates for right, left anterior descending, and LC occlusions, respectively. In conclusion, our results have demonstrated that in clinical practice, the LC artery is the least frequent culprit vessel among patients treated invasively for AMI. Patients with LC occlusion are less likely to present with ST-segment elevation AMI and have emergency PCI. The study results suggest that detection of these patients has been suboptimal, highlighting the need to improve the diagnostic approach toward the detection of an acutely occluded LC artery.
Acute flow-limiting coronary occlusion is associated with the greatest risk of adverse outcomes among patients with myocardial infarction. The presence of ST-segment elevation on the electrocardiogram (ECG) is the criterion used in clinical practice to identify patients with acutely occluded coronary arteries, and current treatment pathways triage accordingly. A major limitation of this approach is that the 12-lead ECG does not detect ST-segment elevation in all patients with acutely occluded culprit arteries and, especially, lacks sensitivity in the left circumflex (LC) territory. Failure to detect an occluded LC artery is not without consequences, because it supplies a significant area of the left ventricle. Current guidelines have recommended placement of 3 additional leads on the posterior wall of the chest to increase the sensitivity of the ECG. Despite this, data from randomized clinical trials of ST-segment elevation acute myocardial infarction (STEMI) have repeatedly shown that LC is the least frequent culprit artery among the patients enrolled. There is a paucity of data on whether the same holds true in routine clinical practice. We hypothesized that, despite the increased awareness of the difficulty of diagnosing an occluded LC artery, patients with infarcts in this territory remain less likely to undergo revascularization. Thus, the aim of the present study was to assess the incidence of LC occlusion in patients with acute myocardial infarction (AMI) treated with percutaneous coronary intervention (PCI), the frequency of ST-segment versus non–ST segment elevation presentation among them, and to correlate the electrocardiographic findings with outcomes.
Methods
The study was conducted among consecutive patients who had undergone PCI from November 2001 through December 2007 with the following inclusion criteria: AMI within 7 days preceding PCI, and a single culprit vessel with either 100% occlusion or ≥90% stenosis with less than Thrombolysis In Myocardial Infarction 3 flow. Patients with graft conduit interventions or left main interventions or those who had undergone elective procedures were excluded.
A total of 1,566 patients with AMI who had undergone PCI for a single culprit vessel were identified. The institutional review board approved the present study.
The diagnosis of AMI before PCI was determined from the final discharge diagnosis in the clinical records. To determine the accuracy of the diagnosis of STEMI versus non–STEMI (NSTEMI), one investigator (PJMB) retrospectively reviewed the preprocedural ECG to confirm the presence or absence of ST-segment elevation. STEMI was diagnosed if ≥1 mm of ST-segment elevation was present in 2 contiguous leads. All other patients with AMI were classified as having NSTEMI. When the ECG before revascularization was not available in the medical records (patients transferred from other hospitals), the description in the medical records from the attending cardiologist who had reviewed the ECG was used to determine the diagnosis. Blood samples for cardiac troponin T levels were collected at admission (before PCI) and 8 and 16 hours after PCI. The peak postprocedure values were used in the present analysis. A sensitive and precise third-generation assay (Elecsys, Roche Diagnostics, Indianapolis, Indiana) was used with an upper limit of normal of <0.01 ng/ml (ninety-ninth percentile).
The number of diseased coronary arteries was defined by the number of major arteries with ≥70% stenosis on visual assessment. Major adverse cardiovascular events were defined as one or more of the following: in-hospital death, Q-wave myocardial infarction, the need for urgent or emergent coronary artery bypass grafting during the index hospitalization, or cerebrovascular accident, defined as transient ischemic attack or stroke. In-hospital deaths included all deaths during the index hospital admission. Procedural success was defined as a reduction of residual luminal diameter stenosis to <20% without in-hospital death, Q-wave myocardial infarction, or the need for emergency coronary artery bypass grafting. Long-term outcomes included all-cause mortality.
Continuous variables were summarized as the mean ± SD if distributed symmetrically or with mild skew and compared using one-way analysis of variance. Other continuous variables that were skewed were summarized as the median (interquartile range) and compared using the Kruskal-Wallis rank sum test. Discrete variables are presented as frequency (percentages) and were compared using Pearson’s chi-square test. Missing values were excluded from the denominator in the calculation of the percentages. Kaplan-Meier methods were used to estimate the survival rates on follow-up with comparisons tested using the log-rank test. All hypothesis tests were 2-sided with a 0.05 type I error rate. Analyses were performed using Statistical Analysis Systems, version 9.1 (SAS Institute, Cary, North Carolina).
Results
The baseline characteristics of the 1,500 patients with AMI are listed in Table 1 , according to the culprit artery. The culprit lesion was located in the right, left anterior descending (LAD), or LC artery in 44.7%, 35.8%, and 19.5% of patients, respectively. Patients with acutely occluded LC arteries were more likely to have undergone PCI >24 hours after the onset of the AMI than those with a culprit lesion in the LAD or right arteries ( Table 1 ). In the entire cohort, the preprocedural troponin values were greater in patients with a LC occlusion.
| Variable | Right (n = 670) | LAD (n = 537) | LC (n = 293) | p Value |
|---|---|---|---|---|
| Age (years) | 64.5 ± 13.3 | 64.4 ± 13.6 | 64.0 ± 13.3 | 0.85 |
| Men | 475 (71%) | 370 (69%) | 225 (77%) | 0.05 |
| Diabetes mellitus | 107 (16%) | 100 (19%) | 53 (18%) | 0.46 |
| Hypertension ⁎ | 414 (67%) | 317 (65%) | 186 (69%) | 0.55 |
| Hypercholesterolemia † | 404 (71%) | 322 (70%) | 182 (74%) | 0.56 |
| Body mass index (kg/m 2 ) | 28.9 ± 5.5 | 29.2 ± 5.8 | 29.5 ± 5.6 | 0.32 |
| Chest pain before procedure | 634 (95%) | 505 (94%) | 279 (95%) | 0.77 |
| Preprocedural shock | 97 (15%) | 76 (14%) | 39 (13%) | 0.87 |
| Peripheral vascular disease | 46 (7%) | 29 (6%) | 27 (9%) | 0.13 |
| Cerebrovascular disease | 59 (9%) | 48 (9%) | 26 (9%) | 0.99 |
| Thrombolytic agents before percutaneous coronary intervention | 103 (16%) | 64 (12%) | 21 (7%) | 0.001 |
| Timing of percutaneous coronary intervention | <0.001 | |||
| ≤24 Hours from acute myocardial infarction | 539 (80%) | 445 (83%) | 206 (70%) | |
| >24 Hours from acute myocardial infarction | 131 (20%) | 92 (17%) | 87 (30%) | |
| Single-vessel disease | 315 (48%) | 309 (59%) | 137 (48%) | <0.001 |
| Angiographic presence of thrombus | 568 (90%) | 426 (85%) | 215 (80%) | <0.001 |
| Preprocedural Thrombolysis In Myocardial Infarction 0 flow | 425 (70%) | 329 (66%) | 182 (71%) | 0.33 |
| Stents per patient | 1.3 ± 0.9 | 1.2 ± 0.7 | 1.0 ± 0.7 | <0.001 |
| Drug-eluting stent use | 296 (44%) | 214 (40%) | 130 (44%) | 0.26 |
| Thrombectomy device use | 72 (11%) | 27 (5%) | 15 (5%) | <0.001 |
| Glycoprotein IIb/IIIa inhibitor use | 540 (81%) | 437 (81%) | 245 (84%) | 0.54 |
| Procedural success | 604 (90%) | 474 (88%) | 250 (85%) | 0.09 |
| Peak preprocedure troponin T ‡ | 0.2 (0.0, 0.8) | 0.3 (0.0, 1.3) | 0.5 (0.1, 1.7) | <0.001 |
| ST-segment elevation presentation | 0.1 (0.0, 0.6) | 0.2 (0.0, 1.2) | 0.2 (0.0, 1.7) | <0.001 |
| Non–ST-segment elevation presentation | 0.5 (0.2, 1.0) | 0.5 (0.2, 1.4) | 0.6 (0.2, 1.5) | 0.053 |
| Peak postprocedure troponin T ‡ | 3.2 (1.4, 6.1) | 4.2 (1.5, 9.7) | 3.1 (1.5, 5.9) | <0.001 |
| ST-segment elevation presentation | 4.0 (1.9, 7.0) | 5.7 (2.6, 11.5) | 4.9 (2.5, 9.4) | <0.001 |
| Non–ST-segment elevation presentation | 1.4 (0.6, 2.7) | 1.3 (0.6, 2.8) | 2.5 (1.1, 4.2) | <0.001 |
⁎ Documented history of hypertension treated with medication.
† History of total cholesterol level >240 mg/dl.
No significant difference was found in the in-hospital mortality (4.4%, 7.4%, and 6.5%, respectively; p = 0.66) or major adverse cardiovascular event (9.2%, 13.9%, and 11.6%, respectively; p = 0.53) rates for patients with right, LAD, and LC occlusions.
A total of 1,077 patients (72%) presented with STEMI and 423 (28%) presented with NSTEMI. Figure 1 demonstrates the relative frequency of STEMI versus NSTEMI presentation according to the culprit artery. Only 127 patients (12%) with STEMI had a culprit lesion in the LC artery compared to 166 patients (39%) presenting with NSTEMI. Figure 2 illustrates the proportion of patients undergoing PCI within 24 hours of presentation according to the culprit vessel and infarct type. PCI was performed within 24 hours in 957 (89%) of 1,077 patients presenting with STEMI and 233 (55%) of the 423 patients presenting with NSTEMI. The pre- and postprocedural troponin T levels according to the culprit vessel and infarct type are summarized in Figure 3 and Table 1 . Of the NSTEMI cohort, those with a LC artery occlusion had the greatest pre- and postprocedural troponin T levels. Of the patients with LC NSTEMI, 78% had Rentrop collateral grade 0 or 1 (no or minimal) flow and 22% had grade 2 or 3 (good) flow. No difference was seen in the 2-year mortality between patients presenting with STEMI and those present with NSTEMI in any of the 3 coronary territories ( Figure 4 ).