Acute Limb Ischemia (Embolus)
NICHOLAS OSBORNE and PETER K. HENKE
Presentation
A 57-year-old man who had an acute myocardial infarction 6 weeks ago, treated with a percutaneous coronary intervention, presents to the emergency department with right lower extremity pain and numbness for 5 hours. The patient also feels light-headed and nauseated but is without chest pain. The patient notes having difficulty moving his right leg. No history of trauma is elicited. Past medical history includes tobacco use and hypertension, but no diabetes or hyperlipidemia. His discharge medications included an aspirin, a beta-blocker, an angiotensin-converting enzyme (ACE) inhibitor, and a diuretic.
On examination, his pulse is 140 beats per minute and irregular, and his blood pressure is 100/60 mm Hg. His abdomen is soft, and he has palpable femoral and pedal pulses in his left leg but no femoral or pedal pulses in his right leg. The right leg is cool and mottled, with decreased sensation and decreased motor function. Laboratory evaluation reveals creatinine, hematocrit, and leukocyte count and coagulation parameters within normal limits. His creatinine kinase is 290, and his lactate is 1.9.
Differential Diagnosis
A pulseless extremity warrants immediate attention. The patient presentation with pain, poikilothermia, pallor, paresthesias, and paralysis represent the classic five Ps of acute limb ischemia (ALI). ALI can be classified by the Society for Vascular Surgery (SVS) ALI grading system (Table 1). This patient represents grade IIB limb ischemia, which may be reversible with prompt intervention.
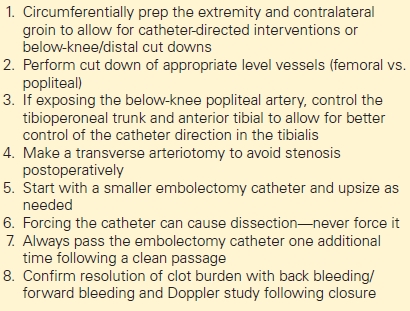
TABLE 1. Key Technical Steps/Potential Pitfalls
Workup
This patient has potential life- and limb-threatening problems with evidence of a new cardiac event (dysrhythmia), as well as ALI. It is common for patients with ALI to have multiple acute medical problems that must be treated appropriately, and saving life before limb is the overriding priority. First and foremost is evaluation and stabilization of his cardiac issues. An electrocardiogram suggests atrial fibrillation but no ST segment elevation or depression. The patient also denies any chest pain, and a rapid troponin I level is within normal limits. Thus, it is unlikely he has suffered a recurrent major myocardial infarction.
The most likely etiology of ALI in this case is a cardiac embolism and is the most common site of origin in general. Diagnostic tests, such as duplex and/or arteriography, may be considered, but minimizing delay in treatment for ALI is essential, because he has evidence of grade IIB limb ischemia. The patient needs revascularization within 1 to 2 hours (total ischemic time ≤6 hours), or he may suffer permanent muscle and nerve damage, rendering a nonsalvageable limb. A duplex or CT angiogram with runoff may be helpful to establish the level of thrombus/embolus, possibly identify a source (aortic thrombus), and demonstrate the presence of disease distal to the occlusion. Arteriography with thrombolysis is an option, but given the patient’s classic history for an arterial thromboembolism (an antecedent cardiac event and normal vascular examination on his contralateral asymptomatic leg), this step may delay reperfusion that could be achieved more readily with surgery. The physical examination is very helpful to localize the site of occlusion in the setting of ALI. In this case, the patient has a diminished femoral pulse on the affected side, suggesting a more proximal lesion.
Diagnosis and Treatment
This patient is suffering from both atrial fibrillation with rapid ventricular response and concomitant ALI. Upon establishing that this patient has ALI, the patient should be started on full-dose intravenous (IV) heparin (80 to 100 U/kg bolus and 18 U/kg/h). Intravenous heparin will not only improve outcomes from his ALI but will both decrease the risk of cardiac emboli from atrial fibrillation (which may also be the etiology of his lower extremity ischemia) and treat potential cardiac ischemia. An aspirin is given orally, as well. The patient’s heart rate is controlled with an IV calcium channel blocker, and he converts to a sinus rhythm. The cardiac issues now seem to be stabilized. Cardiac enzymes are normal.
A CT angiogram of the abdomen pelvis and runoff demonstrates that the patient has an acute thrombus in the left external iliac and common femoral artery with distal reconstitution and three-vessel runoff to the foot. The contralateral side appears completely normal (Figs. 1 to 3).
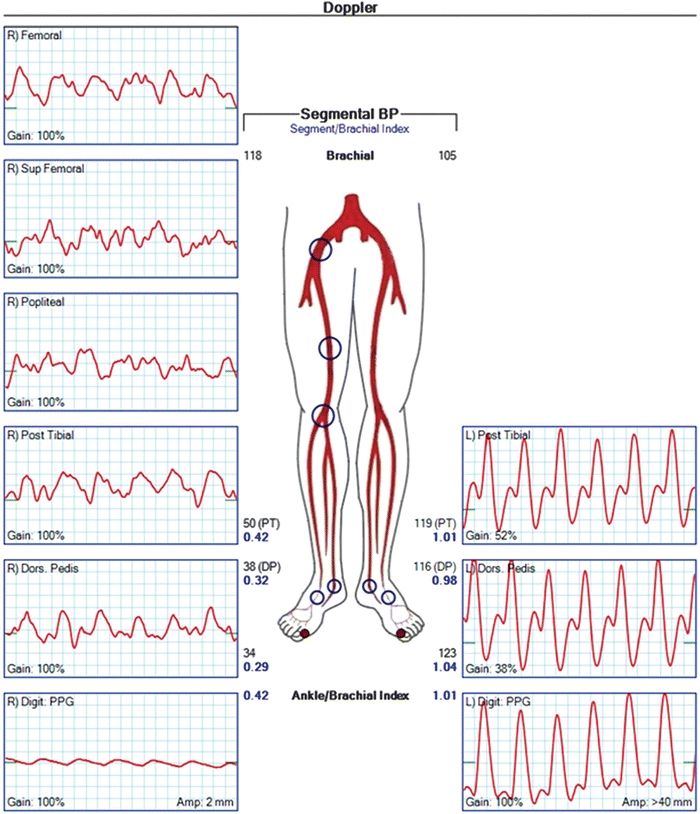
FIGURE 1 Segmental doppler waveforms showing that his waveforms are monophasic from groin all the way to the foot, consistent with an occlusion above the inguinal ligament.



