Acute Iliofemoral Deep Vein Thrombosis
AMIR AZARBAL, GIYE CHOE, and GREG MONETA
Presentation
A 68-year-old woman presents with a 2-day history of a painful, swollen left lower extremity. She is otherwise healthy and has been in her usual state of health until the sudden onset of left leg pain and swelling. She does not smoke or take medications. On exam, her left lower extremity is swollen from her ankle to her thigh and tender to palpation. Her motor and sensory exam is intact, her calf compartments are soft, and she has palpable pedal pulses.
Differential Diagnosis
Sudden onset of painful, unilateral lower extremity swelling represents a lower extremity deep vein thrombosis (LE DVT) until proven otherwise. Provoked DVTs occur in the setting of trauma, surgery, or immobilization. Unprovoked DVTs require investigation of environmental, genetic, and anatomic reasons risk factors for DVT.
Workup
The preferred imaging modality for diagnosis of LE DVT is a duplex ultrasound. d-Dimer blood tests are useful in excluding DVT in cases with low pretest probability of DVT and do not have a role in cases where the clinical presentation is suggestive of DVT. Initiation of anticoagulation should not be delayed until completion of confirmatory testing. Detection of DVT in the iliac veins may be possible using duplex ultrasound, but computed tomography and magnetic resonance venography may be needed to determine the proximal extent of the thrombosis (Fig. 1).
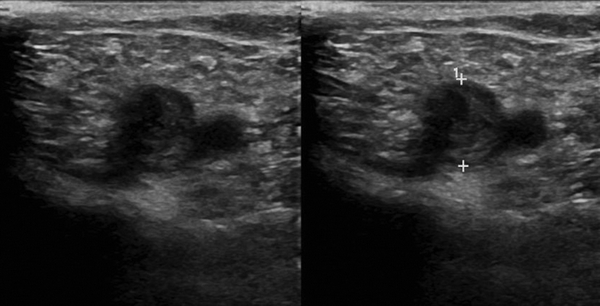
FIGURE 1 Venous duplex ultrasound demonstrating acute deep vein thrombosis of the common femoral vein.
Discussion
Iliofemoral deep vein thrombosis (IFDVT) is a subset of LE DVT that involves the common femoral and/or iliac veins. Immediate pain, swelling, paradoxical stroke, respiratory compromise, and full cardiopulmonary collapse after a pulmonary embolism (PE) can all arise without warning. Venous insufficiency, venous claudication, postthrombotic syndrome (PTS), and chronic thromboembolic pulmonary hypertension (CTPH) can plague patients for the rest of their life. IFDVTs occur more commonly on the left side, and many series also report a higher incidence of IFDVT in women as compared to men.
Virchow’s triad of venous stasis, endothelial injury, and hypercoagulability are commonly named risk factors of LE DVT. IFDVTs have a fourth potential precipitating factor, anatomy. In the absence of precipitating factors causing IFDVT, a hypercoagulable disorder workup and investigation of anatomic causes of IFDVT are warranted. The most common cause of iliac vein compression is May-Thurner syndrome (MTS). MTS describes the mechanical compression of the left common iliac vein by the overlying right common iliac artery. The chronic compression may result in reactive intimal changes that can cause typical intimal “spurs” or webs, which can lead to IFDVT. Other anatomic derangements that fit in the category with MTS include pelvic radiation changes, postsurgical changes, tumor compression, and postthrombotic iliac vein occlusion (Fig. 2).
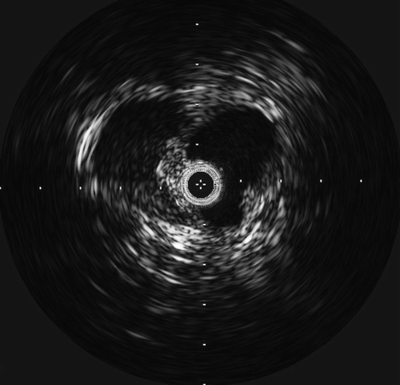
FIGURE 2 Intravascular ultrasound demonstrating an intimal web within the left common iliac vein.
Treatment
Anticoagulation
Systemic anticoagulation remains the cornerstone of treatment for IFDVT. Treatment with anticoagulation is based on a single randomized trial published in 1960, showing that 1.5 days of heparin and just 14 days of oral vitamin K antagonism markedly reduced recurrent PE and mortality. Current recommendations for the treatment of DVT are provided by the American College of Chest Physicians and rigorously reviewed and updated every few years. Treatment of iliofemoral DVT falls under the recommendations for proximal DVT and includes the following:
- Initiation of parenteral anticoagulation such as low molecular weight heparin (LMWH) or fondaparinux and oral vitamin K antagonist without delay and continuation of parenteral agent for at least 5 days and until INR > 2.0 on two separate reads (1B)
- Three months of therapy for provoked DVT with transient risk factor
- Continued therapy past 3 months for unprovoked DVT and acceptable bleeding risk (2B)
While prolonged anticoagulation can decrease the incidence of PTS and recurrent DVT, the benefit of prolonged anticoagulation must be weighed against the increased risk of bleeding. It is important to maintain therapeutic anticoagulation levels as subtherapeutic anticoagulation is associated with risk of recurrence and subsequently PTS.
The use of LMWH for 3 months followed by oral vitamin K antagonism is also reasonable and has some data supporting this regimen is associated with reduced PTS.
Newer oral anticoagulants are now available and emerging as viable alternatives to warfarin for treatment of acute DVTs. Rivaroxaban, dabigatran, and apixaban have been demonstrated in randomized control trials and a systematic review to be as effective as warfarin in preventing overall death, death from PE, and recurrent DVT and PE. Rivaroxaban, edoxaban, and apixaban are direct factor Xa inhibitors. Rivaroxaban and edoxaban are dosed once daily, while apixaban is dosed twice daily. Dabigatran is a direct thrombin inhibitor that is dosed twice daily.
While anticoagulation is quite effective at preventing PE and death, long-term venous function is quite poor. IFDVTs treated with anticoagulation have recanalization rates of about 30% and even worse functional outcomes, with greater than 80% of patients demonstrating abnormal venous function after treatment.
Ambulation
Evidence shows that early ambulation is safe and likely beneficial for patients with LE DVT. According to CHEST guidelines, early ambulation is recommended over bed rest (2C). A number of randomized trials have examined this issue and are summarized in two meta-analyses, both of which demonstrated no increased risk of PE or adverse event. None of the studies that composed the meta-analyses were specific to IFDVT, and rates of IFDVT were not specifically reported in the studies; however, it is unlikely that a study focusing on IFDVT would change these recommendations for early ambulation.
Compression
The first randomized trial of compression stockings showed a 50% reduction in PTS as judged by a nonvalidated scale. A second randomized trial and two meta-analyses have also shown similar decreases in PTS. However, the most recent and largest randomized trial of compression stockings, the SOX trial, did not show any benefit in cumulative incidence or severity of PTS with the use of compression stockings for 2 years after an episode of first proximal DVT. One criticism of this study is that compliance was poor, with only 56% of patients using compression stockings more than 3 days a week. Even before the results of the SOX trial were published, the most recent ACCP guidelines downgraded its recommendation for compression stockings to a 2B level. While the data for compression stockings preventing PTS are not very robust, compression stockings are generally included in the standard of care for patients with DVT due to their low cost and high safety profile and that they often reduce pain.
Endovascular Therapy
Evidence continues to emerge to support an aggressive approach to clearance of IFDVT such as catheter-directed thrombolysis (CDT) and percutaneous mechanical thrombectomy (PMT). A large randomized trial and a meta-analysis have shown better outcomes in terms of PTS occurrence, venous patency, and venous reflux for CDT compared to conventional therapy. The precise technical aspects of this have yet to be standardized, which is part of the reason the ACCP guidelines continue to formally recommend anticoagulation alone over CDT (grade 2C). In cases of IFDVT secondary to iliac vein compression by the overlying iliac artery, consideration should be given to stenting of the compressed iliac vein. There are no randomized data to support the use of venous stents to decrease the incidence of PTS or prevent DVT recurrence; however, the generally poor prognosis of IFDVTs and the good initial results seen with iliac vein stents have made this treatment approach popular.
Case Conclusion
The patient was started on therapeutic LMWH. Duplex US confirmed a left-sided IFDVT. A discussion regarding the risks and benefits of CDT was held, and the decision was made not to proceed with endovascular therapy. The patient was maintained on LMWH, started on warfarin, and discharged home. LMWH was continued until her INR was therapeutic on two separate readings. She was also prescribed 30 to 40 mm Hg compression stockings and given instruction on early ambulation and leg elevation. A complete review of systems and review of health maintenance was not concerning for underlying malignancy. After 3 months of anticoagulation, the risks and benefits of continued anticoagulation were discussed with the patient. Given her low bleeding risk and the fact that she had an unprovoked proximal DVT, she was continued on warfarin therapy indefinitely.



