Acute Dyspnea
Christopher M. Walker, MD
DIFFERENTIAL DIAGNOSIS
Common
Pneumonia
Pulmonary Edema
Pulmonary Embolism
Pneumothorax
Pleural Effusion
Aspiration
Asthma/COPD Exacerbation
Less Common
Lobar Collapse
Septic Embolism
Pericardial Disease
Rare but Important
Acute Interstitial Pneumonia
Pulmonary Hemorrhage
Fat Embolism
Interstitial Lung Disease Exacerbation
Acute Hypersensitivity Pneumonitis
Acute Eosinophilic Pneumonia
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Review focuses on intrathoracic causes of dyspnea presenting within minutes to days
Helpful Clues for Common Diagnoses
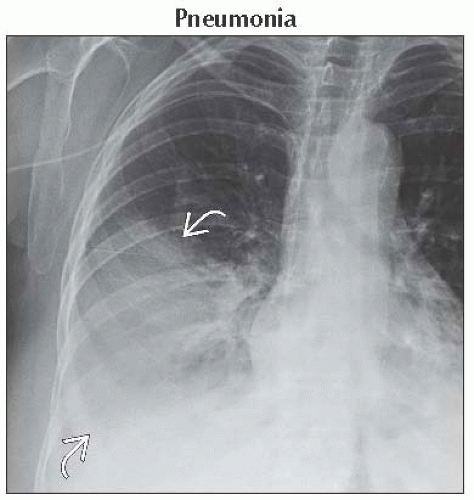
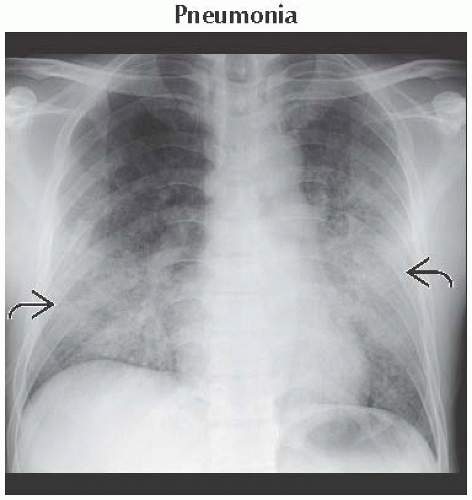
Pneumonia
Symptoms of infection
Lobar or segmental lung consolidation
± pleural effusion
Pulmonary Edema
Pulmonary venous hypertension with transudation of fluid
Radiographs and CT
Smooth interlobular septal thickening (Kerley B lines)
Fissural thickening
Dependent distribution
± pleural effusions
Pulmonary Embolism
CTA: Filling defect is diagnostic
“Railroad track” or “doughnut” signs
Document signs of right heart strain
RV/LV chamber size ≥1, reflux of contrast into IVC, or leftward bowing of interventricular septum
Pneumothorax
Spontaneous
Rupture of apical bleb or bulla
Young, tall, and thin male smokers
Association with emphysema, asthma, infection, lung fibrosis, or cystic lung disease
Recurs in 50% of patients
Traumatic
Chest trauma or mechanical ventilation
Pleural Effusion
Exudative effusions
Causes include infections, malignancy, connective tissue diseases, and asbestos exposure
Pleural thickening and enhancement seen in 60%
Ultrasound depicts septations and heterogeneous echotexture
Transudative effusions
Common in congestive heart failure, renal disease, and hypoalbuminemia
Aspiration
Most common in right lower lobe
Secondary to more vertical orientation of right mainstem bronchus
Pleural effusion is uncommon
Asthma/COPD Exacerbation
Flat diaphragms from lung hyperinflation
Exacerbation usually does not cause new radiographic findings
Associated complications
Pneumonia
Pneumothorax
Pneumomediastinum
Atelectasis
Helpful Clues for Less Common Diagnoses
Lobar Collapse
Signs of volume loss
Mediastinal shift
Fissural displacement
Crowding of vessels
Diaphragmatic elevation
Occurs secondary to
Central obstructing mass or nodule in outpatients
Mucus plug in inpatients
Septic Embolism
Multiple bilateral lower lobe predominant peripheral nodules
± central cavitation
Most common in intravenous drug abusers
Pericardial Disease
Pericardial effusion
Rapid fluid accumulation secondary to malignancy or infection
Acute pericarditis
Pericardial thickening ≥4 mm ± pericardial effusion
Contrast enhancement of thickened pericardium
Helpful Clues for Rare Diagnoses
Acute Interstitial Pneumonia
Acute respiratory distress syndrome without identifiable cause
Viral respiratory syndrome followed by rapid respiratory decline
Bilateral patchy lung consolidation and ground-glass opacity
Most commonly affects dependent lung
50% mortality
Pulmonary Hemorrhage
Ground-glass opacity or patchy/diffuse consolidation
± sparing of subpleural lung
Pleural effusions are rare
Important historical clue is presence of hemoptysis or anemia
Causes
Pulmonary-renal syndromes, vasculitis, anticoagulation, drug reactions, and collagen vascular disease
Fat Embolism
Usually secondary to long bone fracture
Classic clinical triad
Petechial rash, altered mental status, and hypoxia
Small centrilobular and subpleural lung nodules
Nonspecific bilateral ground-glass opacity without zonal predominance
Interstitial Lung Disease Exacerbation
Rapid deterioration in presence of known interstitial lung disease
Must exclude infection (Pneumocystis) and congestive heart failure
Ground-glass opacity or consolidation superimposed on interstitial lung disease pattern
Acute Hypersensitivity Pneumonitis
Occurs with large inhaled antigen exposure
Middle and lower lung consolidation secondary to acute lung injury
± centrilobular nodules of ground-glass opacity
± mosaic perfusion and expiratory air-trapping
Acute Eosinophilic Pneumonia
Fever with rapidly progressing respiratory distress
Eosinophils in serum and lavage fluid
Rapid response to steroids
Radiographic progression similar to pulmonary edema
Bilateral reticular opacities and Kerley B lines
Lower lobe consolidation, small pleural effusions
Image Gallery
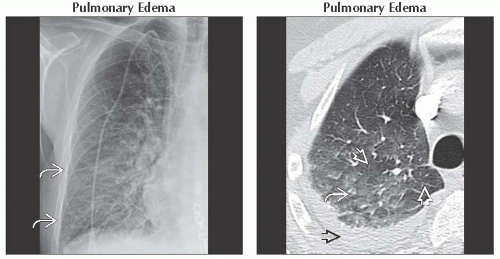 (Left) Frontal radiograph shows multiple lower lobe septal lines or Kerley B lines
 , which represent thickening of interlobular septa. Note vascular indistinctness without alveolar filling. (Right) Axial CECT shows dependent ground-glass opacity , which represent thickening of interlobular septa. Note vascular indistinctness without alveolar filling. (Right) Axial CECT shows dependent ground-glass opacity  with lobular sparing with lobular sparing  secondary to differing lobular perfusion. Note right pleural effusion secondary to differing lobular perfusion. Note right pleural effusion  . New onset edema is a presenting sign of myocardial infarction in 50% of patients, as in this case. . New onset edema is a presenting sign of myocardial infarction in 50% of patients, as in this case.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|