7.3 CLINICAL PRESENTATION
Presentations of unstable angina are based on the duration and intensity of angina as graded by the Canadian Cardiovascular Society classification scheme (class 0 – asymptomatic; class 1 – angina with strenuous exercise; class 2 – angina with moderate exertion; class 3 – angina with mild exertion; and class 4 – angina at any level of exertion). NSTEMI generally presents as more intense prolonged angina or angina equivalent.
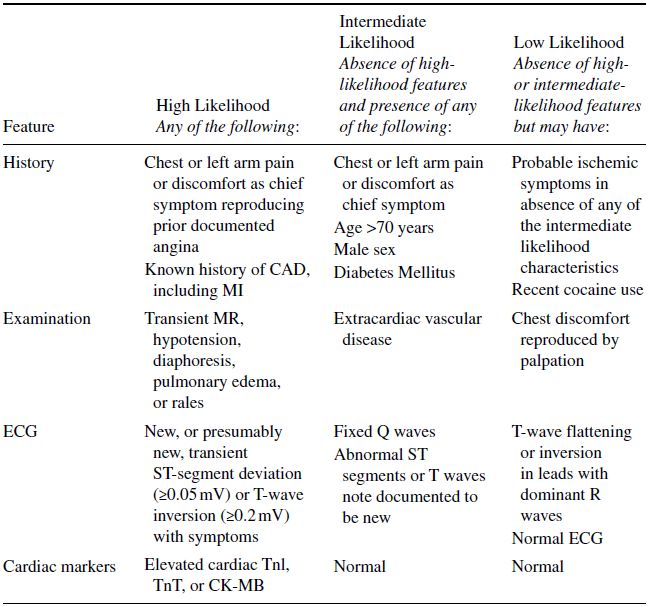
The ACS spectrum requires early recognition of symptoms, as well as the appropriate classification of the likelihood of acute ischemia (Table 7.1), as it has substantial clinical and economic consequences. The five most important factors derived from the initial history, ranked in order of importance, are: (1) the nature of the anginal symptoms; (2) prior history of CAD; (3) gender; (4) age; and (5) the number of traditional risk factors present. Classically, the chest discomfort is described as a pressure sensation arising in the substernum that often radiates to the left upper extremity and neck or jaw, exacerbated by activity or emotional stress, and relieved by rest and/or nitroglycerin. Associated symptoms include diaphoresis, dyspnea, nausea, vomiting and unexplained fatigue. Atypical presentations are more common among women and the elderly.
ACS, as associated with coronary heart disease, has well established major risk factors, including smoking, family history, adverse lipid profile, diabetes mellitus, and elevated blood pressure. However, the presence or absence of these risk factors is far less important than symptoms, ECG findings, and cardiac biomarkers.
The physical examination is focused on identifying possible precipitating causes of myocardial ischemia and to assess hemodynamic consequences. Findings indicating large areas of ischemia and high risk that demand a more aggressive management pathway include: diaphoresis; cool extremities; tachycardia; third or fourth heart sounds; murmurs; basilar rales; and hypotension. Other conditions that may be considered in the differential diagnoses of ACS should also be evaluated for, including unequal pulses ± aortic regurgitation (aortic dissection), pericardial friction rub (acute pericarditis), and diminished breath sounds (pneumothorax).
Table 7.1 Likelihood Signs and Symptoms Represent ACS Secondary to CAD (Source: Adapted from Anderson et al. 2007. With permission of Wolters Kluwer Health).
7.4 EVALUATION AND DIAGNOSTIC STUDIES
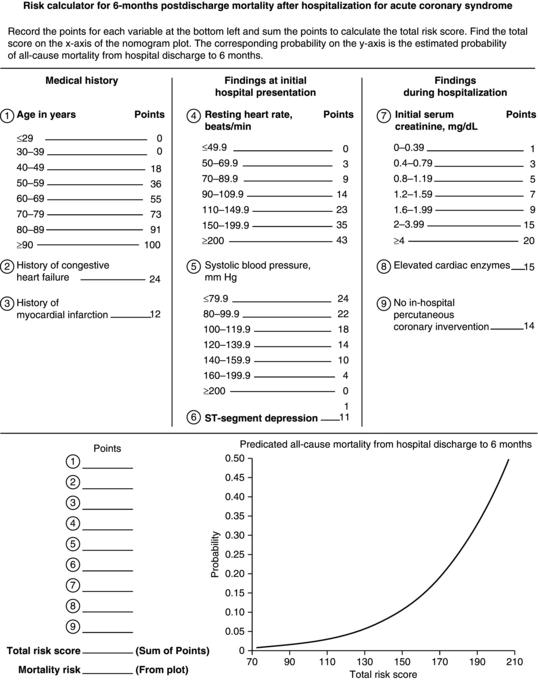
Several risk assessment schemes have been developed in evaluating patients with UA/NSTEMI and are an integral prerequisite to decision-making. The Global Registry of Acute Coronary Events (GRACE) risk tool uses eight variables to predict in-hospital mortality (and death or MI) in patients with STEMI, NSTEMI or UA, and is used to guide treatment type and intensity (Figure 7.1). As a part of this assessment, several diagnostic studies also are instrumental in its evaluation. An online tool is available for calculating the GRACE risk tool: http://www.outcomes-umassmed.org/GRACE/acs_risk/acs_risk_content.html
Figure 7.1 GRACE prediction score sheet and nomogram for all-cause mortality (Source: Anderson et al. 2007. Reproduced with permission of Wolters Kluwer Health).
7.4.1 Electrocardiography
Specific pattern characteristics and magnitude of pattern abnormalities increase the likelihood of ACS. Findings associated with UA/NSTEMI include: (a) new or dynamic ST-segment depression (>0.5 mm); (b) T-wave inversion (≥3 mm); and (c) nonspecific ST-segment changes (≤0.5 mm) and T-wave changes (≤2 mm). The latter is much less specific and may also be related to drugs (e.g. phenothiazines, tricyclic antidepressants, digitalis, etc.), hyperventilation, repolarization abnormalities associated with left ventricular hypertrophy or conduction disturbances. Serial ECG tracings or continuous ST-segment monitoring early on during hospitalization are encouraged as myocardial ischemia may be dynamic.
7.4.2 Cardiac Biomarkers
Cardiac biomarkers detect myocardial necrosis and are recommended to be measured for all patients presenting with signs and symptoms suggestive of ACS. Cardiac troponins (cTnI or cTnT) allow for high accuracy, sensitivity and specificity in diagnosing myocardial injury. Recent expert groups have defined myocardial necrosis as an elevation of troponin above the 99th percentile of normal. Myocardial infarction, which is necrosis related to ischemia, is further defined by the elevation of troponin and one of the following criteria: ischemic ST and T-wave changes, new left bundle-branch block, new Q-waves, PCI-related marker elevation, or positive imaging for loss of viable myocardium. Cardiac troponins are detectable about 6 hrs after myocardial injury and measurable for up to 2 weeks. Mortality risk is directly proportional to the level of troponin elevation and its prognostic information is independent of other clinical and ECG risk factors. Creatine kinase-MB, the prior standard marker for the diagnosis of MI, is less sensitive and less specific than the cardiac troponins. However, because of its shorter half-life, CK-MB is useful to detect eventual infarct extension and recurrent MI. Myoglobin is a nonspecific, very early marker that can be used to provide high-negative predictive value for MI.
Besides markers of myocardial necrosis, markers of inflammation are also under investigation. C-reactive protein (CRP) levels appear to be related to long-term mortality after ACS in an independent and additive fashion to troponin levels. The role of other markers, such as amyloid A, interleukin-6, fibrinogen, plasminogen activator inhibitor-1 (PAI-1), and B-type natriuretic peptide (BNP), are yet undefined.
7.4.3 Non-Invasive Testing
A chest radiograph should be used to evaluate for other causes of chest pain and screen for pulmonary congestion, implicating a worse prognosis in ACS. Echocardiography
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


