10.3 CLINICAL MANIFESTATIONS AND EVALUATION
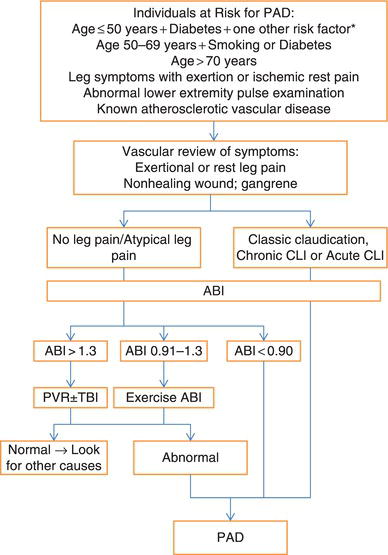
The diagnostic work-up of patients with suspected PAD can be seen in Figure 10.1.
10.3.1 Signs and Symptoms
A history should include a vascular review of symptoms to assess for claudication, rest pain, walking impairment and impaired wound healing in the lower extremities. Claudication must be differentiated from pseudoclaudication and other nonvascular causes of claudication (see Table 10.1). Sedentary patients may not experience symptoms until exerted by a 6-minute walk test, on a treadmill or with repeated chair raises or leg elevation. Screening for the presence of PAD has been recommended in some high-risk groups (see Table 10.2), but its relevance for hospitalists is less clear. The severity of stenosis is correlated with the amount of exercise required to elicit claudication symptoms. Pain symptoms typically present one segment below the level of obstruction. They are gradual in onset and relieved rapidly with rest. Distal aortic disease manifests with gluteal claudication, iliac disease with thigh pain and superficial femoral artery (SFA) disease with calf claudication. When impotence and diminished femoral pulses are combined with gluteal claudication, this is known as Leriche Syndrome. Critical limb ischemia (CLI) presents with rest pain, non-healing ulcerations, or gangrene.
Physical examination is focused on the vascular system and requires careful evaluation for signs of acute or chronic peripheral ischemia with the patient’s shoes and socks removed. Attention should be paid to the quality of carotid and peripheral pulses (femoral, popliteal, posterior tibial and dorsalis pedis) with regard to upstroke, amplitude and presence of bruits. Other signs of PAD include hair loss, coolness, skin pallor, scaling, and ulcerations and dystrophic nails. The abdomen should be palpated for evidence of an aortic aneurysm and blood pressure checked in both arms.
Figure 10.1 Diagnosis of Peripheral Artery Disease (PAD). ABI, Ankle-brachial index; CLI, Critical limb ischemia. *Risk factors include: cigarette smoking, diabetes mellitus, hypertension, hyperlipidemia, hyperhomocysteinemia, chronic renal insufficiency. (Source: Adapted from Hirsch AT, Haskal ZJ, Hertzer NR, et al. 2006. With permission of Elsevier).
10.3.2 Diagnostic Testing
The diagnostic evaluation for PAD starts with ABIs. Table 10.3 lists the advantages and disadvantages of additional imaging modalities that are used in conjunction with ABIs.
Ankle/Brachial Index (ABI)
Measurement of ankle and brachial blood pressures is an accurate and practical noninvasive laboratory test for detecting PAD. The ABI, which is the ratio of these two measurements of blood pressure, can be performed at the bedside with ease and correlates well with disease severity (Table 10.4). It should be measured in both the right and left ankle, with the highest systolic pressure compared with the highest systolic pressure obtained in either upper extremity. A resting ABI of less than 0.90 is diagnostic of PAD with 95% sensitivity and 99% specificity for excluding PAD. Its sensitivity and specificity are increased by simultaneous Doppler velocity waveform (VWF) measurements. Based on the principle that blood flow accelerates through stenotic areas, Doppler VWF uses the peak systolic and end-diastolic velocities through an arterial segment to estimate the degree of stenosis. “Exercise” ABI can be useful in unmasking significant PAD in patients with a high index of suspicion but normal resting ABIs (e.g. isolated iliac stenosis). With treadmill exercise testing, a decrease in ABI of 15–20% from baseline is diagnostic of PAD. With noncompressible, calcified vessels (most commonly in patients with diabetes, renal failure or advanced age), the ABI is less useful and measuring a toe-brachial index (TBI) may be warranted, with values less than 0.7 considered diagnostic for PAD. The ABI with Doppler VWF can be effectively used as a serial test to monitor progression of PAD.
Table 10.1 Differentiation of Vascular Claudication from Pseudoclaudication (Nonvascular Causes).
Table 10.2 Populations to screen for peripheral artery disease (PAD).
| Populations to screen for PAD |
| Age ≤50 + diabetes + one other risk factor* Age 50–69 + diabetes or smoking Age ≥70 + abnormal pulse exam or known atherosclerosis |
*Risk factors include: cigarette smoking, diabetes mellitus, hypertension, hyperlipidemia, hyperhomocysteinemia, chronic renal insufficiency.
Table 10.3 Noninvasive and Invasive Diagnostic Imaging for Peripheral Artery Disease.
Table 10.4 Ankle Brachial Index Calculation and Interpretation.
| Interpretation of calculated index >1.30 – non-compressible vessels 1.00–1.29 – normal 0.91–0.99 – borderline 0.71–0.90 – mild obstruction 0.41–0.70 – moderate obstruction 0.00–0.40 – severe obstruction |
Pulse Volume Recordings (PVR)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


