Acute Aortic Occlusion in a Hostile Abdomen
MARK G. DAVIES
Presentation
A 70-year-old male inpatient complains of sudden onset of paralysis in both his legs for 4 hours. He had been admitted with small bowel obstruction and is 15 days after a laparotomy and lysis of adhesions. This was considered a difficult operation, and the patient has developed a midline enterocutaneous fistula. He has a previous history of an extended left colectomy for Duke’s stage C colonic adenocarcinoma 2 years previously and has completed adjuvant chemotherapy. He has a past history of bilateral lower extremity claudication at 100 yards. He has hypertension controlled by two antihypertensive medications, is a non–insulin-dependent diabetic, and has chronic renal insufficiency (eGFR of 58 mL/min/1.73sqm). On examination, the patient is noted to be in mild respiratory distress and unable to move his legs. His upper extremity power and sensation are intact. He is noted to have an irregularly irregular heart rate and to be hypotensive (BP 90/50), tachypneic (30/m), and oliguric (less than 10 mL/hour for the last 4 hours). Examination of the peripheral pulses notes absent pulses in the right and left legs. Femoral pulses were documented as being present, but diminished on his admission physical examination. His legs are cold and pale. He has no motor or sensory function from L1/L2 dermatomes distally. No continuous-wave Doppler signals were identified.
Differential Diagnosis
The differential diagnosis in this case is that of a saddle embolus or acute aortic occlusion. The history of previous claudication would suggest preexisting aortoiliac disease and allow one to suspect acute aortic occlusion rather than saddle embolism. Both require emergent therapy but with different approaches. The presentation is atypical, but is also serious as the patient has paralysis likely due to cauda equina ischemia, and rapid revascularization must be considered.
Workup
This patient is in shock and had very ischemic limbs. An arterial blood gas and a serum chemistry panel are obtained, and an angiogram is arranged. On the blood gas and serum chemistry, the patient has a new-onset metabolic acidosis. This raises the suspicion of mesenteric vessel involvement. Having obtained informed consent, the patient is placed under general anesthesia. In the hybrid operating room, the right arm, right chest, abdomen, and both legs are prepared and draped in a standard fashion to form a sterile field. An angiogram is obtained through a right brachial cut down to ensure no vessel injury and speed closure. The emphasis of the angiogram is to define the visceral vessels, the infrarenal aorta, and bilateral runoff. The angiogram demonstrates intrarenal aortic occlusion with heavy calcifications suggestive of chronic disease. The visceral vessels are intact (Fig. 1). There is reconstitution of the common femoral vessels bilaterally. Prior to right brachial sheath removal, the right subclavian was studied and it was normal.
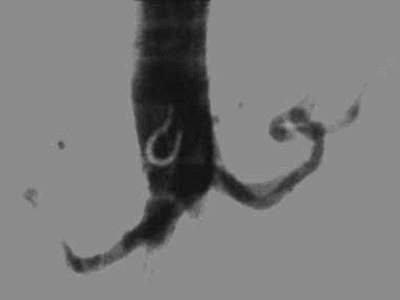
FIGURE 1 Angiogram of the aorta with AP views demonstrating acute aortic occlusion. A lateral view confirms patent celiac and superior mesenteric vessels.
Case Continued
Prior to and during the angiogram, the patient is resuscitated and prepared for surgery and is heparinized (80 units/kg, IV) to achieve an activated clotting time (ACT) of greater than 250 seconds.
Diagnosis and Recommendation
The patient has a hostile abdomen, an enterocutaneous fistula, and a left colectomy, and as such, a direct transabdominal approach or a retroperitoneal approach would be very difficult. Options in this patient are to attempt endoluminal therapy to reopen one or both iliac vessels. If one iliac is open, a femorofemoral bypass is possible. If this fails, the patient should be considered for axillobifemoral bypass grafting. Acute occlusion of the abdominal aorta due to in situ thrombosis is a relatively rare event with a cumulative incidence of 8% (aortic occlusion due to embolic disease has a relative incidence of 15%). It has a mortality rate of over 50%.
Case Continued
Under fluoroscopy, percutaneous access is gained into both common femoral arteries, sheaths are placed, and guide wires are passed retrograde into the aorta. The right passed without difficulty, but the left failed to pass. A rheolytic thrombectomy catheter system, initially using bolus instillation of 5-mg tPA in 50 mL to lace the clot with a thrombolytic and then followed by heparinized saline set to standard mode, is performed. The rheolytic thrombectomy catheter is passed over the wire multiple times without adequate restoration of antegrade flow. At this stage, it is decided to stop and pursue open intervention. Primary stenting using covered stents to pave open one iliac system was considered, but risk of thrombus embolization into the visceral vessels was considered to be high (Fig. 2).
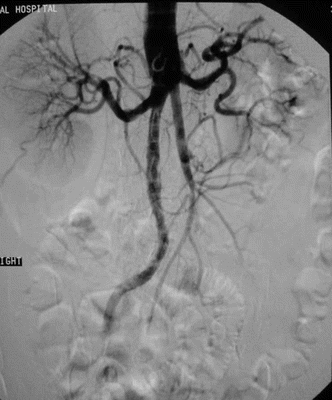
FIGURE 2 Angiogram of the aorta in an AP view demonstrating a channel in the aorta after rheolytic catheter thrombectomy.
Surgical Approach
At this stage, endoluminal intervention cannot be achieved. Bilateral groin cutdowns are performed with care to preserve the femoral artery branches. Following proximal and distal control, Fogarty embolectomies are performed to remove any distal clot and perhaps open up flow proximally to the hypogastric arteries. A right axillobifemoral bypass graft with 8-mm ringed PTFE is performed without difficulty (Table 1). Intraoperative duplex imaging, in order to reduce contrast exposure, confirms adequate distal outflow. The patient receives 25 mg mannitol to induce forced diuresis prior to reperfusion of the lower limbs. Due to the severity of the lower leg ischemia, bilateral four-compartment fasciotomies of the lower extremities are also performed. There are continuous-wave Doppler signals in the anterior and posterior tibial vessels on the foot at the end of the case. Intraoperative labs shows a rising potassium, which peaks at 8.0 and is aggressively treated with fluid diuresis, intravenous glucose, as well as insulin and calcium.
The following potential pitfalls of the operation as it is routinely conducted can be considered (Table 1):
1. Insufficient laxity in subclavian anastomosis and graft to prevent anastomotic distraction: When the subclavian anastomosis should be constructed, there will be sufficient laxity to allow for shoulder extension and the graft should be routed laterally before being directed caudally.
2. Not using ringed graft material to prevent compression: There is a high risk of compression of the graft along the lateral course of the body wall, and as a result, a ringed graft will prevent compression.
3. Angle of the takeoff of both ends of the femorofemoral graft: It is important to set up the femorofemoral anastomoses so that there is a downward angle of the anastomoses to prevent preferential flow or steal.
4. Care to avoid left Internal Mammary Artery (IMA) occlusion in a post-CABG patient: In left-sided dissections of the subclavian artery, care should be taken to identify and preserve the IMA in patients who are post CABG as occlusion of the vessel can lead to significant myocardial events.
5. Competitive flow in iliac system resulting in occlusion: If an axillobifemoral bypass is placed and there is native flow in the iliac system, a competitive flow situation can occur leading to occlusion of the most vulnerable element of the axillobifemoral bypass (the contralateral side).
6. Dissection with Fogarty embolectomy catheter: Care should be taken when placing and withdrawing a Fogarty embolectomy catheter as overpressurization of the balloon can lead to intimal dissection or disruption. If there is an inability to access a specific vessel over the wire Fogarty, embolectomy balloons should be considered.



