29 Access Management and Closure Devices
 Introduction
Introduction
The steady increase in percutaneous interventional procedures for the treatment of cardiovascular diseases in a variety of vascular territories is associated with closer attention to access-site management. The more aggressive level of anticoagulation used during therapeutic procedures requires the achievement of safe and reliable hemostasis of the access site. Coronary interventions are usually performed by the femoral approach; however, to reduce complications and increase patient comfort, radial access is increasingly used and is becoming the preferred access site by many interventionalists.1 Patients undergoing the femoral approach are usually immobilized overnight, which may result in significant discomfort because of increased back pain and the need for analgesics. Noncompliance of patients regarding strict bed rest after the procedure has been reported to be a substantial factor for femoral complications. During the last decade, there has been a rapid increase in the percutaneous treatment of aortic aneurysms, aortic dissections, and aortic valve replacement using much larger sheaths that require special attention to the access site. The most common catheterization problem involves the access site.2,3 Additionally, major access-site complications increase the length of hospital stay and medical costs. Moreover, vascular complications are also associated with an increased risk of nonfatal myocardial infarction or death in the year following the procedure, in particular when accompanied by significant bleeding.4 The use of manual or mechanical compression was until recently the only way to control bleeding by allowing clot formation at the arteriotomy site. The clinical use of vascular closure devices for rapid hemostasis after femoral access was first reported in 1991. Since then, these devices have improved patient comfort by enabling early ambulation, and their use has decreased the burden of the medical staff. However, they have not produced a reduction in groin complication rates. This chapter summarizes the concepts of arterial access puncture, the use of arterial closure devices, and postprocedural management.
 Planning Access
Planning Access
Retrograde Puncture Technique for the Femoral Artery
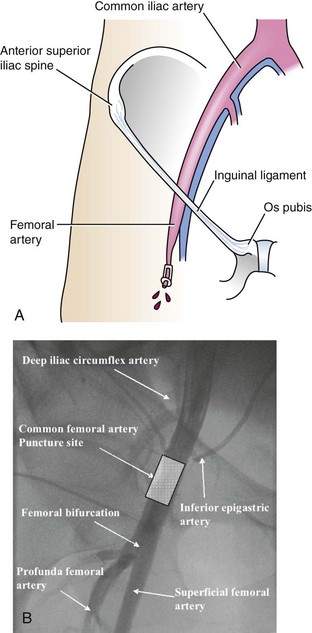
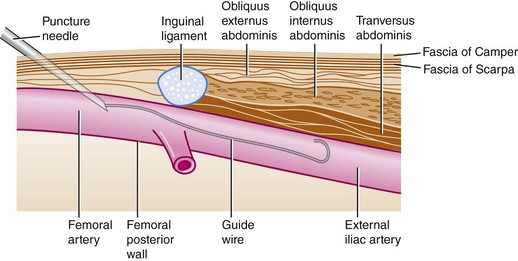
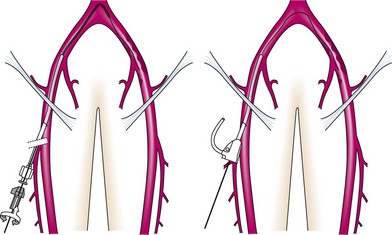
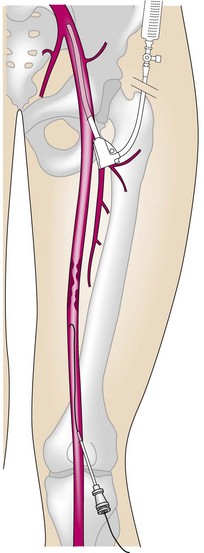
Ideally, the femoral artery is entered about 1 or 2 cm below the inguinal ligament (Fig. 29-1). If cannulation of the artery is too low, the chance of entering the superficial femoral artery rather than the common femoral artery is increased. This entry site may predispose to dissection, arterial occlusion, pseudoaneurysm, bleeding, and arteriovenous fistula formation. Entering the artery above the inguinal ligament may lead to problems in compressing the artery against the inguinal ligament, thus increasing the risk of hematoma formation and favoring retroperitoneal hemorrhage. The use of femoral closure devices is contraindicated in higher or lower femoral punctures. The other important aspect is careful puncture of only the anterior wall of the femoral artery with open-bore needles, which have the advantage of demonstrating blood return immediately. Appropriate vascular hemostasis can be achieved with the use of manual compression or femoral closure devices (Fig. 29-2). A reduction in the sheath size was presumed to result in fewer access complications, but there was no clear association with a decrement in the bleeding rate. Retrograde femoral access can be considered the standard technique for coronary, renal, iliac, and crossover for contralateral femoral interventions (Fig. 29-3). Endovascular repair of abdominal and thoracic aortic aneurysms has become the standard of care for anatomically appropriate patients. All the devices developed to date are deployed through relatively large (12- to 24-Fr) sheaths. Moreover, transcatheter aortic valve implantation is a rapidly emerging treatment option for patients with aortic valve stenosis and high surgical risk. Different access routes have been proposed, including transapical, transsubclavian, and transfemoral, with percutaneous transfemoral being preferred because it is the least invasive and potentially nonsurgical. However, vascular access-site complications due to the large-bore (18- to 24-Fr) delivery catheters remain an important clinical issue, particularly with respect to elderly patients. Traditionally, this access has required arterial exposure with open cut-down; but with the development of suture-mediated arterial closure devices, there is an increasing trend toward percutaneous endovascular repair. This is an effective and safe approach in a select group of patients. The procedure should be performed in a sterile operating room environment with the support of vascular surgeons in the event that the closure device should fail to close the arteriotomy. The need for larger sheaths for these interventions requires a meticulous puncture technique in the anterior wall of the common femoral artery.
Puncture Technique for the Radial Artery
Miniaturization of the procedural equipment has led to a revival of the transradial approach. Despite the considerable training needed, this approach remarkably improves patient comfort and decreases bleeding complications, particularly among patients with aggressive anticoagulation regimens. This approach provides an alternative for coronary angiography and angioplasty and for vertebral and internal mammary interventions. It is addressed in Chapter 30.
Puncture Technique for the Brachial Artery
Brachial access is an alternative technique that can be used for coronary, renal, and lower limb interventions. However, radial access is usually preferred because of a higher rate of complications at the brachial access site, such as artery occlusion or hematoma. Puncture of the brachial artery should be performed in its distal part above the antecubital fossa, where the artery is relatively superficial. At this level, after sheath removal, the artery can be compressed against the humerus to obtain hemostasis (Fig. 29-4). Direct puncture of the axillary artery, which has been performed in the past, has largely been abandoned.
Anterograde Puncture Technique for the Femoral Artery
The anterograde puncture technique provides more direct access to many lesions in the femoropopliteal segment and the infraglenoidal arteries. It allows for the use of a lower volume of contrast and provides stronger support for chronic occlusions of the superficial femoral artery. However, anterograde puncture is technically far more challenging. Although a high puncture of the common femoral artery is required to allow enough space in which to navigate the guidewire into the superficial femoral artery, suprainguinal puncture should be avoided because of the higher risk of retroperitoneal bleeding (Fig. 29-5). Injection of contrast through the needle usually helps to identify the femoral bifurcation anatomy.
Puncture Technique for the Popliteal Artery
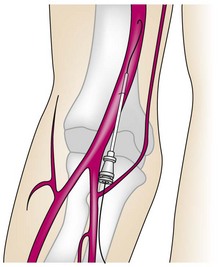
Transpopliteal access becomes useful when the superficial femoral artery cannot be crossed using other techniques. The patient is placed in a prone position. The puncture is performed with the assistance of road-map fluoroscopy after the injection of contrast from an ipsilateral femoral sheath (Fig. 29-6). Particular attention should be paid to achieving complete hemostasis after intervention. The incidence of access-site complications is potentially higher with transpopliteal access than with conventional techniques.5
Transapical Left Ventricular Puncture
Transapical left ventricular puncture gives direct access to the left ventricle; although it was frequently used in the past for diagnostic reasons, it has largely been abandoned in favor of transvenous-transatrial or retrograde access because these routes are associated with fewer complications. Nevertheless, there are multiple clinical circumstances where direct transapical access is required for diagnostic or interventional indications, including access to the left ventricle in the setting of double mechanical valves, inaccessible percutaneous mitral paravalvular leak repair, complex congenital heart disease, percutaneous valve implantation, and many others.6,7 Percutaneous transthoraxic puncture is appealing for an interventional cardiologist but can be complicated by lung puncture, resulting in pneumothorax or hemothorax due to damage to the internal mammary and subcostal arteries or persistant leak after sheath withdrawal. Damage to the coronary artery can be avoided by doing selective coronary angiography before puncture. However, most of these complications can be minimized by puncturing “under direct vision” after a minithoracotomy. Transthoracic or transesophageal cardiac ultrasound is useful in guiding the operator to the access site either for direct puncture or to perform the minithoracotomy.