Alterations in cardiac rate
Cardiac arrhythmias result from either of two mechanisms: (a) automatic tachycardias – alterations in the rate of discharge of pacemakers at the atrial, junctional, or ventricular level, or (b) re-entry mechanisms, occurring solely within the atria (primary atrial tachyarrhythmias) or the ventricles (some types of ventricular tachycardia), or from re-entry circuits involving atria, ventricles, junctional tissue, and abnormal atrial-to-ventricular connections (atrioventricular tachyarrhythmias).
Atrial and atrioventricular arrhythmias
Sinus arrhythmia
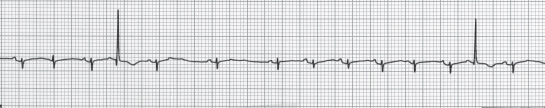
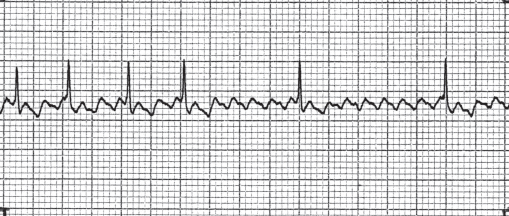
Sinus arrhythmia is a normal variation of sinus rhythm (Figure 10.1). It describes the normal increase in cardiac rate with inspiration and the slowing with expiration. Sometimes with expiration, nodal escape occurs.
Figure 10.1 Electrocardiogram of sinus arrhythmia. Each QRS complex is preceded by a P wave, but the interval between each P wave is variable, usually changing with the respiratory cycle.
Premature atrial systole
Premature atrial systole (or contractions, PACs) (Figure 10.2) occur commonly in the fetus and young infant less than 2 months of age but uncommonly in older children; they arise from ectopic (and automatic) atrial foci. On the electrocardiogram this condition is recognized by a P wave with an abnormal shape which differs in contour from the patient’s usual P waves. The P waves occur earlier than normal, so prematurely, in fact, that the atrioventricular node is completely refractory and a QRS complex does not occur. PACs that occur during partial atrioventricular (AV) node refractoriness may be conducted aberrantly, mimicking multiform premature ventricular contractions (PVCs). PACs occurring after the AV node has ceased to be refractory are conducted normally, resulting in a narrow QRS complex. No treatment is required.
Sinus tachycardia
The normal sinoatrial node can discharge at a rapid rate of up to 210 beats per minute (bpm) in response to some stimuli such as fever, shock, atropine, or epinephrine. The increased heart rate does not require treatment, but the tachycardia should be considered a clinical finding that requires diagnosis and perhaps treatment of the root cause.
Paroxysmal supraventricular tachycardia
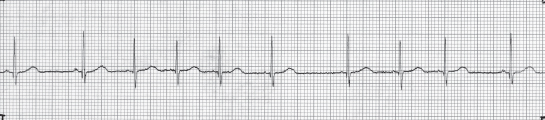
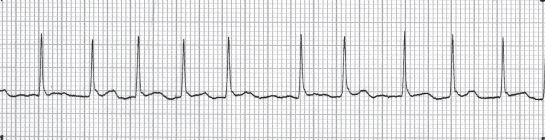
Paroxysmal supraventricular tachycardia (SVT, PSVT, PAT), often occurring with minimal or no symptoms, rarely leads to death if untreated. Typically, a previously healthy infant develops poor feeding, sweating, irritability, and rapid respiration. If the arrhythmia is unrecognized and untreated, congestive cardiac failure may progress to death in 24–48 hours. Recognition of arrhythmia is not difficult when examining the heart. The measured heart rate of 250–350 bpm (Figure 10.3) is remarkably regular, showing no variation when the child breathes, cries, or becomes quiet.
Figure 10.3 Electrocardiogram of supraventricular tachycardia. A regular narrow-QRS tachycardia without easily seen P waves. Heart rate 220 bpm.
The prognosis is excellent because many infants have no underlying cardiac malformation and recurrent episodes are rare or infrequent and are well tolerated, if of short duration. A few infants with coexistent Ebstein’s malformation and/or Wolff–Parkinson–White syndrome, however, may have repeated episodes of supraventricular tachycardia.
Orthodromic reciprocating atrioventricular tachycardia (ORT)
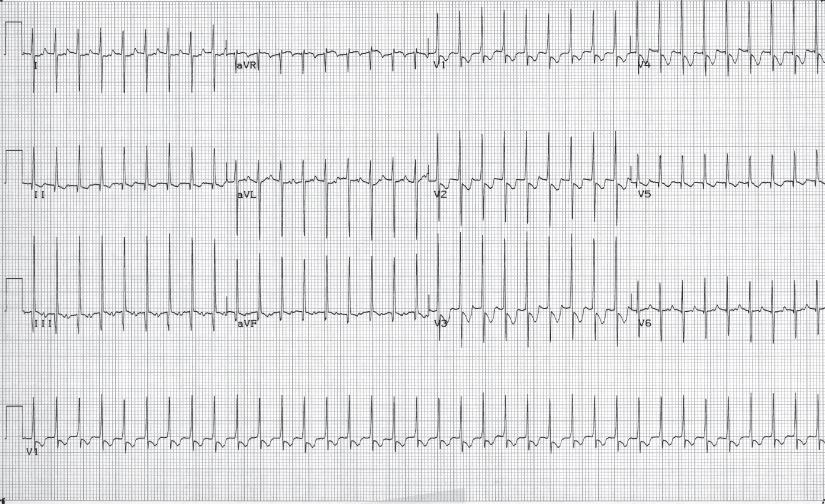
The mechanism of this type of tachycardia is virtually always re-entry via an accessory pathway between the atria and ventricles (Figure 10.4). Normally, only one electrically conductive pathway, the penetrating bundle of His, exists between the atria and ventricles. In more than 95% of fetuses, infants, and young children with SVT, an abnormal accessory connection exists between the atria or ventricles, a possible vestige of the multiple connections that exist in the embryonic cardiac tube before separate cardiac chambers are formed.
Figure 10.4 Mechanisms of supraventricular tachycardia. Orthodromic reciprocating tachycardia (ORT) is the most common in children. An abnormal accessory connection (AC) with the atrioventricular node (AVN) and the atria and ventricles constitutes a re-entrant circuit. In atrioventricular node re-entry tachycardia (AVNRT), the circuit includes two pathways within the AVN and also the atria and ventricles. Both types result in a regular narrow-QRS tachycardia without discernible P waves. Primary atrial tachycardia (e.g. atrial flutter) originates in the atria (true SVT) and conducts via the AVN to the ventricles – in this case, in a 2:1 ratio. P waves may or may not be seen. The lower panel allows simultaneous comparison of the surface ECG with electrograms recorded in the atria and ventricles. In each type, the sinoatrial node (SAN) is suppressed because of the more rapid SVT.
This accessory connection together with the AV node, the atria, and the ventricles may create a large re-entrant circuit (Figure 10.4). Impulses may conduct normally via the AV node (orthodromic conduction) but pass retrograde to the atria via the accessory connection when the AV node is refractory. Then the impulse passes from atria through the AV node, to the ventricles, then to the atria via the accessory connection, as the sequence is repeated. This creates orthodromic reciprocating tachycardia (ORT), the most common mechanism for childhood SVT. Because the tachycardia is not truly supraventricular but actually atrioventricular and is dependent on four components – atria, AV node, ventricles, and accessory connection – any of these components can be altered slightly to terminate the tachycardia. In practical terms, the AV node is the component most amenable to intervention by vagal stimulation or medication such as adenosine.
Since conduction is antegrade at all times, the QRS complex appears normal during the tachycardia. The tachycardia rate slows with age, being up to 300 bpm in neonates and 200 bpm in adolescents. Because of the length of the re-entrant circuit, the P wave may be more clearly seen following the QRS complex often best in lead V1.
Atrioventricular nodal re-entry tachycardia (AVNRT)
The second most common tachycardia mechanism involves a small re-entrant circuit within or near the AV node itself (Figure 10.4). It can be thought of as an acquired form of SVT, since it has never been reported in children less than 4 years of age but does occur in half of adults with SVT. As in ORT, the tachycardia depends on atria, ventricles, and a fast and a slow pathway within the AV node. This atrioventricular tachycardia is called atrioventricular nodal re-entry tachycardia (AVNRT). The electrocardiogram shows a regular, narrow-QRS tachycardia similar in appearance to ORT. Conversion is best accomplished by altering AV node conduction via vagal stimulation or medication.
Differentiation of AV re-entrant tachyarrhythmias
ORT must be distinguished from AVNRT at the time of catheter ablation, but clinically and by noninvasive means this can be challenging. In a practical sense, the medical treatments of ORT and AVNRT are often the same or very similar. The location of the P wave in relation to the QRS complex is a valuable diagnostic sign, being close in AVNRT and further removed in ORT. In most children, visualization of the retrograde P wave is difficult if not impossible by a standard surface ECG. (Other than by electrophysiologic catheterization, techniques such as transesophageal electrocardiography, i.e. recording of an atrial electrogram by positioning an electrode catheter within the esophagus behind the left atrium, can allow good visualization of the P wave and the R–P interval). Clinically, AVNRT may be more frequent, occurring several times per day, and the tachycardia rate varies between episodes by a greater degree than with ORT.
Atrial flutter
In atrial flutter, the atrial rate may be between 280 and 400 bpm with a 2 to 1, or greater, degree of AV block, so that the ventricular rate is slower than the atrial rate (Figure 10.4). On the electrocardiogram, the atrial activity does not appear as distinct P waves; instead, it has a sawtooth appearance (Figure 10.5).
Figure 10.5 Electrocardiogram of atrial flutter. Regular P waves with less than 1:1 atrioventricular conduction. Atrial rate >300 bpm.
This arrhythmia can occur in infants without an underlying condition or in children with conditions such as dilated cardiomyopathy, Ebstein’s malformation, or rheumatic mitral valvar disease that leads to a greatly enlarged left atrium.
Digitalization usually slows the ventricular rate by slowing the atrioventricular node, but rarely does it result in conversion. Cardioversion (synchronized with the R wave to avoid induction of dangerous ventricular rhythms) with very low energy (usually 0.25 Joule/kg) converts the rhythm to a sinus mechanism.
Atrial fibrillation
Atrial fibrillation is associated with chaotic atrial activity at a rate of more than 400 bpm. Distinct P waves are not seen, but atrial activity is evident as small, irregular wave forms on the electrocardiogram (Figure 10.6). The ventricular response is irregular. This arrhythmia results from conditions that chronically dilate the atria. Hyperthyroidism is a rare cause in childhood. Medication such as digoxin, beta-blockers, or calcium channel blockers are indicated to slow the ventricular response. Cardioversion may require a high energy (1–2 J/kg), although biphasic shocks are often successful at lower energy compared with monophasic shocks.
Figure 10.6 Electrocardiogram of atrial fibrillation. The wavy isoelectric line reflects the irregular and rapid atrial activity. Typically, the ventricular rate is “irregularly irregular.”
Reinitiation of atrial fibrillation is common, especially with underlying structural heart disease or cardiomyopathy. Antithrombotic therapy, usually with coumadin, is often used to minimize the risk of embolic stroke. In some patients, particularly those with complex postoperative problems, atrial fibrillation may be refractory to antiarrhythmic medication. Such patients may be candidates for a surgical or catheter (radiofrequency ablation) procedure to create multiple linear scars within the atria to prevent atrial fibrillation from becoming sustained (Maze procedure). In other patients, tolerance of chronic atrial fibrillation may be achieved by control of ventricular rate, using a variety of techniques, including medication or AV node ablation plus pacemaker implantation.
Other primary atrial tachyarrhythmias
Primary atrial tachycardia arises from a specific automatic (not re-entrant) atrial focus and does not involve the SA or AV nodes or ventricles in maintaining the abnormal rhythm. Various types may involve one or more foci, and have been termed atrial ectopic tachycardia, ectopic atrial tachycardia or chaotic atrial tachycardia. Occurring at any age during childhood, atrial tachycardia is an incessant or frequently occurring tachycardia and often presents as a tachycardia-induced cardiomyopathy. The heart rate varies, being as high as 300 bpm in infants and ranging from 150 to 250 bpm in children. The rate can vary abruptly. P-wave morphology is usually abnormal and depends on the location of the ectopic focus. P waves are generally observed and the PR interval is normal. Sinus tachycardia is the major condition from which this tachyarrhythmia must be distinguished.
Because of the natural history, treatment depends on age. In infants and young children, the tachycardia often resolves, so these patients are treated with medications. Amiodarone or flecainide is preferred. After a few years, medications can be withdrawn if the tachycardia has resolved. For older children, ablation of the ectopic focus is successful and may need to be performed acutely if the child is ill and has poor ventricular function.
Junctional arrhythmias
These ectopic (automatic) arrhythmias arise from the atrioventricular node; they are called nodal or junctional premature beats or tachycardia.
Premature junctional contractions (PJCs)
The QRS complex is normal because the impulses propagate along the normal conduction pathway. The P waves may appear with an abnormal form shortly before the QRS complex, may be buried within the QRS complex, or may follow the QRS complex.
Junctional ectopic tachycardia (JET)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree