Nonadherence to cardiovascular medications such as statins is a common, important problem. Clinicians currently rely on intuition to identify medication nonadherence. The visit-to-visit variability (VVV) of low-density lipoprotein (LDL) cholesterol might represent an opportunity to identify statin nonadherence with greater accuracy. We examined the clinical and pharmacy data from 782 members of the Boston Medical Center Health Plan, seen at either the Boston Medical Center or its affiliated community health centers, who were taking statins and had ≥3 LDL cholesterol measurements from 2008 to 2011. The LDL cholesterol VVV (defined by the within-patient SD) was categorized into quintiles. Multivariate logistic regression models were generated with statin nonadherence (defined by the standard 80% pharmacy refill-based medication possession ratio threshold) as the dependent variable. The proportion of statin nonadherence increased across the quintiles of LDL cholesterol VVV (64.3%, 71.2%, 89.2%, 92.3%, 91.7%). Higher quintiles of LDL cholesterol VVV had a strong positive association with statin nonadherence, with an adjusted odds ratio of 3.4 (95% confidence interval 1.7 to 7.1) in the highest versus lowest quintile of LDL cholesterol VVV. The age- and gender-adjusted model had poor discrimination (C-statistic 0.62, 95% confidence interval 0.57 to 0.67), but the final adjusted model (age, gender, race, mean LDL cholesterol) demonstrated good discrimination (C-statistic 0.75, 95% confidence interval 0.71 to 0.79) between the adherent and nonadherent patients. In conclusion, the VVV of LDL cholesterol demonstrated a strong association with statin nonadherence in a clinic setting. Furthermore, a VVV of LDL cholesterol-based model had good discrimination characteristics for statin nonadherence. Research is needed to validate and generalize these findings to other populations and biomarkers.
The visit-to-visit variability (VVV) of cardiovascular risk factors, such as low-density lipoprotein (LDL) cholesterol, in clinical practice has been thought to be due to random variation or measurement error. Although several physiologic mechanisms have been posited to contribute to VVV, medication nonadherence could be a key contributor. Indirect evidence for an effect of nonadherence on VVV came from a meta-analysis of the effect of different blood pressure medications on VVV. That meta-analysis found that diuretics and calcium channel blockers were associated with lower VVV than were angiotensin-converting enzyme inhibitors and β blockers. This observation was thought to possibly result from medication adherence, although few data have tested this hypothesis. These observations created the possibility that the VVV of a biomarker such as LDL cholesterol, which has a strong correlation to a medication effect such as that from statins, might demonstrate an observable phenomenon of VVV according to differences in statin adherence. If established, the VVV of LDL cholesterol could be used to detect and trigger interventions to address statin nonadherence in clinical settings in which pharmacy claims data are not electronically integrated, such as currently the case in the large majority of the United States. To test this hypothesis, we conducted analyses using an integrated pharmacy claims and clinical database from a large urban population of adult medical patients to determine the independent association of VVV in LDL cholesterol and statin adherence.
Methods
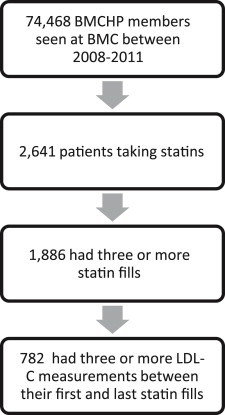
The study sample was patients enrolled in the Boston Medical Center (BMC) Health Plan from 2008 to 2011 who received care from BMC or any of 8 affiliated community health centers during that time. The patient data were drawn from the Massachusetts Health Disparities Repository (MHDR), which uses the Informatics for Integrating Biology and the Bedside system to aggregate de-identified data for BMC and BMC Health Plan. The MHDR currently contains >650 million electronic health record-based data elements (medications, diagnoses, laboratory test results, visit dates, and clinical observations) and claims data (including filled prescriptions) from the BMC Health Plan for the >1,200,000 subjects who received ≥1 clinical service at BMC or any of 8 affiliated community health centers during the past 10 years. We used the Informatics for Integrating Biology and the Bedside to access data from the MHDR to examine 74,468 BMC Health Plan members seen at BMC during the sample period. From this group, we limited our analysis to the 2,641 patients taking statin medications from 2008 to 2011. Of those taking statins during this period, 1,886 had ≥3 prescriptions filled; of those with ≥3 statin prescriptions filled, 782 had ≥3 LDL cholesterol measurements between their first and last statin fulfillment dates ( Figure 1 ). The LDL cholesterol measurements that were outside the 0.1th and 99.9th percentiles were top and bottom coded to those values. If multiple LDL cholesterol measures existed for the same date (n = 68 dates), an average of the same day measurements was used as a part of the VVV estimation, and it was counted only once toward the 3-measure minimum. The primary exposure variable was the VVV of LDL cholesterol between the first and last statin fulfillment dates during the 3-year study period. The VVV of LDL cholesterol was defined as the within-patient SD during the study period. LDL cholesterol VVV was categorized into quintiles. The within-patient mean LDL cholesterol was calculated by averaging the LDL cholesterol measures during the study period.
The primary outcome was medication adherence to statins, as determined from the medication possession ratio (MPR). The MPR, also known as the proportion of days covered, is calculated as the sum of the days’ supply of the medication (in this case, a statin) obtained between the first prescription fill and the last, divided by the total number of days in this period. This method was used as the main measure of medication adherence. The MPR was calculated using all statin fills during the study period. The statin MPR was dichotomized as nonadherent and adherent according to the standard cutoff of <80% and ≥80%, respectively.
Covariate data of previously reported weak correlates of statin adherence were obtained from the MHDR Informatics for Integrating Biology and the Bedside portal. The covariates included age at the first statin fill during the study period, gender, race/ethnicity (white, black, Hispanic, other), total number of outpatient visits during the study period, mean LDL cholesterol level, number of LDL cholesterol measurements during the study period, number of days between the first and last statin prescription fills, and the diagnosis of diabetes mellitus (“International Classification of Diseases, 9th revision,” codes 250.0x to 250.9x), ischemic heart disease (codes 410.0x to 414.9x), hypertension (codes 401.0x to 405.0x), chronic liver disease (codes 571.0x to 571.9x), or cerebrovascular disease (codes 430.0x to 438.9x) at any point during the study period.
Descriptive data are reported as percentages or the mean ± SD, as appropriate. All variables were examined for normality and outliers. Bivariate associations between covariates and quintiles of LDL cholesterol VVV, and between covariates and statin adherence, were tested through chi-square statistics for categorical variables and the Wilcoxon rank-sum test for continuous variables.
Multivariate logistic regression models were used to examine the association between VVV of LDL cholesterol and statin nonadherence (MPR <80%). We performed an unadjusted model with the VVV of LDL cholesterol alone and an adjusted model that included age at the first statin fill, gender, race/ethnicity (define 2 paragraphs previously), and within-patient mean LDL cholesterol. Additional covariates were examined for inclusion in the models but were not included because they did not materially affect the results (number of LDL cholesterol measurements during the study period and diagnosis of diabetes mellitus, ischemic heart disease, hypertension, chronic liver disease, or cerebrovascular disease during the study period). For all logistic regression models, the odds ratios and 95% confidence intervals (CIs) were calculated. The significance level was set at p <0.05. The performance of each model for predicting the statin MPR of <80% was assessed by plotting the receiver operating characteristic curve and calculating the C-statistic (area under the receiver operating characteristic curve).
Sensitivity analyses were conducted by dichotomizing the VVV of LDL cholesterol quintiles into the first and second quintiles versus the third through fifth quintiles. We also substituted quintiles of VVV of total cholesterol for quintiles of VVV of LDL cholesterol and dichotomized statin MPR as <50% versus ≥50%. We also conducted analyses restricted to the first 3 LDL cholesterol measures to examine the effect of patients with greater numbers of LDL cholesterol measures. We also conducted an analysis, withdrawing the first LDL cholesterol measure as an indirect control for the effect of a “first statin fill,” in which there should be a substantial variation between LDL cholesterol measures; an effect that might dilute the relation between adherence and LDL cholesterol VVV. We also repeated all analyses using the coefficient of variation instead of the SD as the measure of VVV and using a continuous measure of LDL cholesterol VVV. Data analyses were conducted using SAS/STAT software, version 9.2, of the SAS System for Windows (SAS Institute, Cary, North Carolina).
Results
After restricting the data set to patients with ≥3 statin pharmacy claims and 3 LDL cholesterol values within the dates of the first and last statin fill, the final analytic data set contained 782 patients. The average within-patient mean LDL cholesterol for our sample was 109.2 ± 32.9 mg/dl.
The VVV of LDL cholesterol ranged from 0.6 to 79.6 (mean 21.7 ± 13.1). The distribution by gender, race, number of outpatient visits, and days between the first and last statin fills across VVV quintiles was equal ( Table 1 ). The mean age at the first statin fill declined as the quintile of VVV increased, with a more significant decline with increasing VVV quintile when age was dichotomized at 55 years (data not shown). The proportion of the sample with diabetes also significantly declined as the quintile of VVV increased. The number of LDL cholesterol measurements (mean 4.6 ± 1.8) and the within-patient mean LDL cholesterol level both increased significantly with increasing LDL cholesterol VVV.
| Variable | Quintile | p Value | ||||
|---|---|---|---|---|---|---|
| ≤10.4 (n = 157) | >10.4–≤16.4 (n = 156) | >16.4–≤23.0 (n = 157) | >23.0–≤32.3 (n = 155) | >32.3 (n = 157) | ||
| Gender | ||||||
| Female | 77 (49%) | 87 (56%) | 77 (49%) | 91 (59%) | 94 (60%) | 0.15 |
| Male | 80 (51%) | 69 (44%) | 80 (51%) | 64 (41%) | 63 (40%) | |
| Age at first prescription fill (yrs) | 5 ± 8 | 53 ± 7 | 53 ± 7 | 52 ± 8 | 52 ± 8 | <0.01 |
| Race | ||||||
| White | 39 (25%) | 44 (28%) | 36 (23%) | 32 (21%) | 34 (22%) | 0.29 |
| Black | 59 (38%) | 59 (38%) | 66 (42%) | 58 (38%) | 58 (40%) | |
| Hispanic | 18 (12%) | 25 (16%) | 28 (18%) | 37 (24%) | 32 (21%) | |
| Other | 39 (25%) | 27 (17%) | 27 (17%) | 27 (18%) | 29 (19%) | |
| Outpatient visits (n) | 46 ± 40 | 46 ± 39 | 45 ± 36 | 49 ± 58 | 42 ± 31 | 0.78 |
| Diagnosis | ||||||
| Diabetes mellitus | 108 (69%) | 117 (75%) | 104 (66%) | 95 (61%) | 88 (56%) | <0.01 |
| Coronary heart disease | 38 (24%) | 36 (23%) | 31 (20%) | 30 (20%) | 33 (21%) | 0.8 |
| Hypertension | 148 (94%) | 145 (93%) | 142 (91%) | 134 (87%) | 129 (82%) | <0.01 |
| Chronic liver disease | 7 (5%) | 6 (4%) | 6 (1%) | 13 (8%) | 11 (7%) | 0.27 |
| Cerebrovascular disease | 17 (11%) | 16 (10%) | 14 (9%) | 12 (8%) | 17 (11%) | 0.86 |
| Framingham risk index | 0.17 ± 0.11 | 0.19 ± 0.13 | 0.20 ± 0.14 | 0.16 ± 0.13 | 0.19 ± 0.14 | <0.01 |
| Low-density lipoprotein measurements (n) | 4.1 ± 1.6 | 4.5 ± 1.6 | 4.7 ± 1.6 | 4.9 ± 2.0 | 5.0 ± 2.2 | <0.01 |
| Within-patient mean low-density lipoprotein (mg/dl) | 89 ± 26 | 101 ± 32 | 109 ± 27 | 115 ± 27 | 133 ± 34 | <0.01 |
| Interval between first and last fill dates (days) | 983 ± 360 | 1,027 ± 351 | 979 ± 361 | 979 ± 355 | 1,003 ± 343 | 0.67 |
| Statin medication possession ratio | <0.01 | |||||
| <80% | 101 (64%) | 111 (71%) | 140 (89%) | 143 (92%) | 144 (92%) | |
| ≥80% | 56 (36%) | 45 (29%) | 17 (11%) | 12 (8%) | 13 (8%) | |
No significant association was found between statin nonadherence and gender, number of outpatient visits, co-morbidities, number of LDL measurements, or number of days between the first and last statin fills ( Table 2 ). Younger age was associated with statin nonadherence. Race also demonstrated a significant relation with statin nonadherence, with blacks having a greater proportion of statin nonadherence than all other race groups. A greater within-patient mean LDL was significantly associated with statin nonadherence.
| Variable | Statin MPR | p Value | ||
|---|---|---|---|---|
| <80% (n = 639) | ≥80% (n = 143) | Overall (n = 782) | ||
| Gender | 0.36 | |||
| Female | 353 (55%) | 73 (51%) | 426 (55%) | |
| Male | 286 (45%) | 70 (49%) | 356 (46) | |
| Age at first prescription fill (yrs) | 52 ± 8 | 55 ± 7 | 53 ± 8 | <0.01 |
| Race | <0.01 | |||
| White | 135 (21%) | 50 (36%) | 185 (24%) | |
| Black | 258 (41%) | 42 (30%) | 300 (39%) | |
| Hispanic | 122 (19%) | 18 (13%) | 140 (18%) | |
| Other | 118 (19%) | 31 (22%) | 149 (19%) | |
| Outpatient visits (n) | 45 ± 41 | 47 ± 44 | 46 ± 42 | 0.96 |
| Diagnosis | ||||
| Diabetes mellitus | 422 (66%) | 90 (63%) | 512 (66%) | 0.48 |
| Ischemic heart disease | 137 (21%) | 31 (22%) | 168 (22%) | 0.95 |
| Hypertension | 568 (89%) | 130 (91%) | 698 (89%) | 0.48 |
| Chronic liver disease | 33 (5%) | 10 (7%) | 43 (6%) | 0.39 |
| Cerebrovascular disease | 62 (10%) | 14 (10%) | 76 (10%) | 0.97 |
| Framingham risk index | 0.18 ± 0.13 | 0.19 ± 0.13 | 0.18 ± 0.13 | 0.24 |
| Low-density lipoprotein measurements (n) | 4.6 ± 1.8 | 4.5 ± 1.8 | 4.6 ± 1.8 | 0.36 |
| Within-patient mean low-density lipoprotein (mg/dl) | 112 ± 33 | 96 ± 29 | 109 ± 33 | <0.01 |
| Interval between first and last fill dates (days) | 1,000 ± 338 | 968 ± 418 | 994 ± 354 | 0.97 |
The prevalence of statin nonadherence increased across greater quintiles of LDL cholesterol VVV (64.3%, 71.2%, 89.2%, 92.3%, and 91.7%). In the unadjusted logistic regression models, a strong positive and significant association was noted between increasing quintiles of VVV and statin nonadherence ( Table 3 ). When adjusted for gender, age at first statin fill, race, and within-patient mean LDL cholesterol, the association was attenuated but remained statistically significant. The inclusion of the number of LDL cholesterol measurements, number of outpatient visits, number of days between the first and last statin fills, or co-morbidities to the model did not appreciably change the association of the VVV of LDL cholesterol and adherence (data not shown).



