Prevention for children with a normal heart
Risk factors for adult-manifest cardiovascular disease
Many risk factors have been identified for the development of atherosclerotic disease of coronary, cerebral, and other arteries. Some factors are more important and/or prevalent in childhood than others, and their impact in adulthood begins with exposure in childhood and adolescence. We discuss factors that are generally regarded to have the greatest preventive benefit if effective modification can be achieved early in life. Several factors are strongly interrelated (e.g. obesity and abnormal lipid and glucose metabolism).
Tobacco
Tobacco use is the single most important independent risk factor for the development of atherosclerotic cardiovascular disease that is purely environmental, and thereby potentially modifiable. Adults who smoke have a two- to fourfold increased risk of myocardial infarction.
Because of the poor rate of recovery from tobacco addiction, prevention of first use of smoking and other tobacco products among children and adolescents is the single most important means of avoiding adverse health effects in adulthood.
The long-term abstinence rate among adults without physician-based intervention is less than 5% and yet with intervention it is only about 40%.
Passive smoking is risky for children, so family members and household contacts should be counseled not to smoke. The cardiovascular risk is related to both dose and duration, and a safe lower limit of passive exposure has not been determined.
Hypercholesterolemia
Coronary atherosclerosis is a highly prevalent problem in developed societies and less common in other cultures, suggesting that diet, lifestyle, and other environmental factors are important. A strong genetic component also influences the metabolism of lipids, which has an important effect on individual disease.
Mechanism of cardiovascular effect
Atheroma, the basic lesion of coronary and other arteriosclerosis, is an erosion of the arterial endothelium capped by a lipid-laden plaque. These plaques may slowly narrow the coronary arterial lumen, leading to intermittent insufficiency of arterial blood flow (creating myocardial ischemia and symptoms of angina). They can also rupture, lead to acute thrombosis and occlusion of the artery, and result in myocardial infarction and/or sudden cardiac death. The exact role of lipids in the initial endothelial injury is unclear. Atheromas are known to begin in childhood; therefore, prevention of adult cardiovascular disease should also begin in childhood.
where TC represents total cholesterol and HDL-C is high-density lipoprotein cholesterol. This equation is invalid if the patient is nonfasting, if abnormal lipoprotein is present (type III; see later), and when triglycerides exceed 400 mg/dL. Current estimates in adults suggest that calculated LDL-C levels vary from measured levels by as much as 25%.
Screening and intervention
The goals of screening include identification of children with familial dyslipidemia (1–2% of patients), secondary causes of hyperlipidemia (1%), and those at highest risk for adult-manifest cardiovascular disease (10–25% of all children).
Screening of blood lipid levels in children has been controversial because of lack of consensus about which children to screen, the age of screening, and the lipid level limits (cut points) at which to consider a patient for further testing or intervention.
One approach has been to risk-stratify children for screening (targeted screening); another is to screen all children (universal screening).
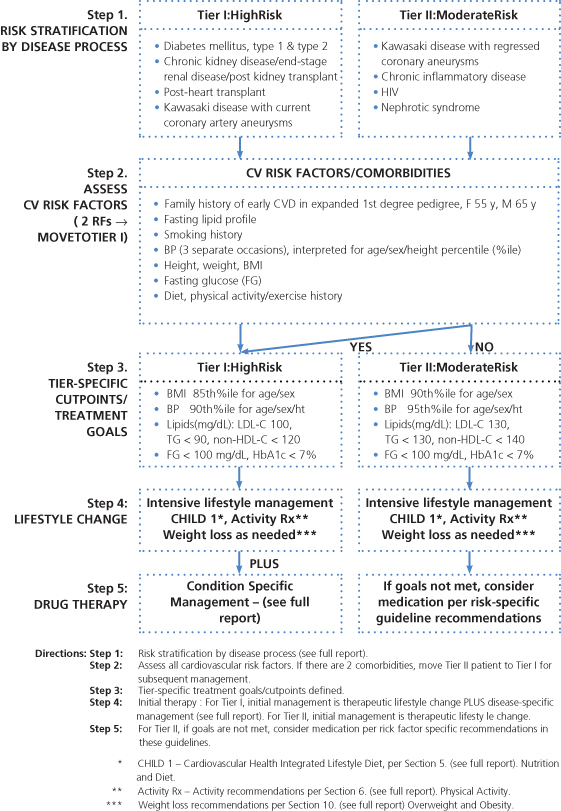
However, risk-stratification is part of both screening strategies. Children and adolescents are evaluated according to their body mass index (BMI), blood pressure, family history, and the presence of conditions associated with increased risk of coronary artery disease, such as diabetes, familial hypercholesterolemia, renal disease, Kawasaki disease, and chronic inflammatory disease such as lupus. Note that those with a high risk (Tier I) have lower values for cut points. For Tier II patients, the cut points are higher (Figure 12.1). Depending on the individual child’s level of risk, differing cut points for lipids, blood pressure, and so on are then targeted for intervention.
Figure 12.1 Risk stratification and management for children with conditions predisposing to accelerated atherosclerosis and early CVD. Source: National Heart, Lung, and Blood Institute, National Institutes of Health, US Department of Health and Human Services. See full guidelines and references in National Heart, Lung, and Blood Institute (2012) The Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents. Full Report, NIH Publication No. 12-7486, National Institutes of Health, Bethesda, MD; www.nhlbi.nih.gov.
Controversy also exists concerning the most appropriate intervention to offer when an affected child is identified. The safety and efficacy of dietary restriction of essential fatty acids on growth and central nervous system development are unknown. The advisability and safety of drug therapy are uncertain. Recent (2012) guidelines have been criticized for placing increased emphasis on drug therapy in children and adolescents. Also, in general, these and earlier guidelines have proved to be complicated and unwieldy in clinical use, and with low adherence by medical providers and parents. Recommendations continue to evolve as more data become available.
- identification of an individual child’s risk factors;
- family history;
- lipid measurement;
- diet and exercise to achieve acceptable lipid levels;
- drug therapy when indicated;
- referral to a lipid specialist when indicated.
Guidelines have been criticized for fixed lipid cutoff values, which, depending on the age of the child at screening, identify not just the top quartile, but up to 75% of children as being at risk. Concerns have been expressed about the number of blood samples required and the potential for a large number of children to experience “medicalization” of a preventive health issue that will not be manifest for decades.
One screening strategy has been to advise universal screening but to restrict it to children 9–12 years old, an age at which childhood lipid levels may best correlate with their adult values; postpubertal lipid levels tend to be lower before rising again to adult levels in late adolescence. It is hoped that those at greatest risk, such as those with familial hypercholesterolemia (FH), can be identified.
Adults in the upper quartile for lipid concentration are at the highest risk for cardiovascular disease. Most of these adults and their children do not have a specific lipid metabolism disorder. Their children tend to be those with lipid levels in the highest quartile and “track” along similar percentiles into their adult years. Screening and preventive measures are designed to identify and improve risk for these 25% of children also.
Blood lipid levels vary by age, gender, and, to some extent, ethnicity. Ethnicity may involve environmental factors (diet and lifestyle may vary between cultures) and also genetic factors.
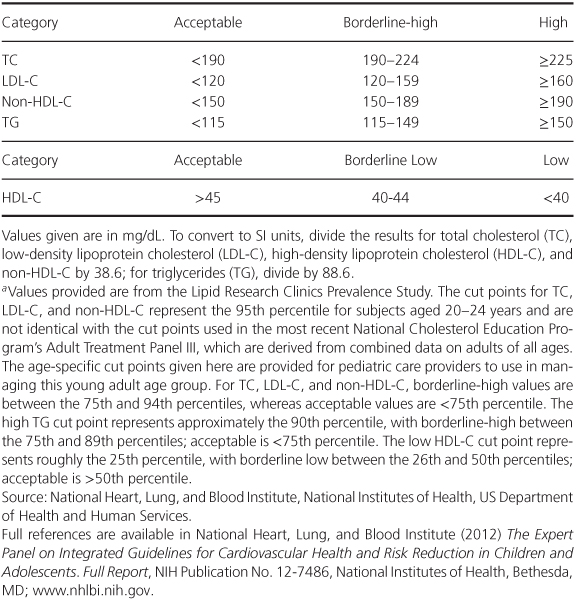
In general, lipid levels in the late teenage years best predict adult levels, but for younger children, the lipid percentile level correlates better with adult percentile rank. Values by age and gender are presented in Table 12.1. Acceptable lipid values have been presented in 2012 NHLBI guidelines (Table 12.2 and Table 12.3). Lipid levels alone do not perfectly predict future coronary artery disease.
Table 12.1 Blood Lipid Levels in a Sample of US Children.
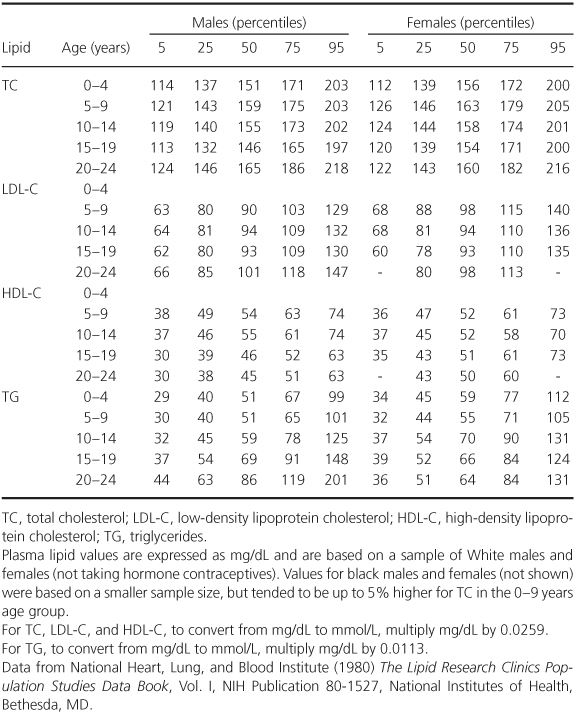
Table 12.2 Acceptable, Borderline-High, and High Plasma Lipid, Lipoprotein, and Apolipoprotein Concentrations (mg/dL) for Children and Adolescentsa.
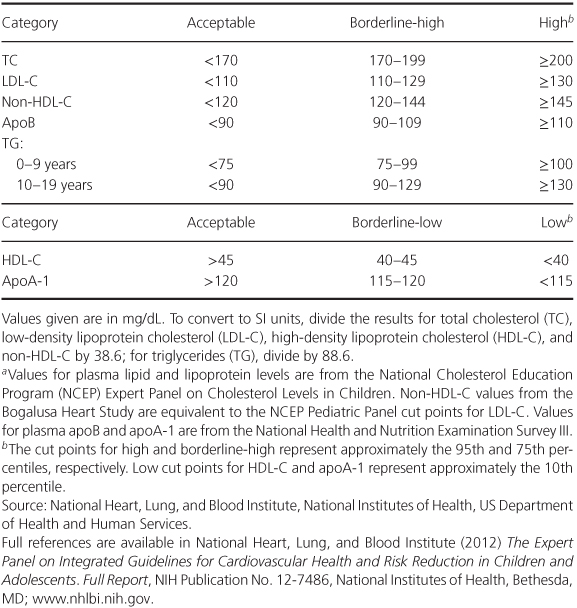
Table 12.3 Recommended Cut Points for Lipid and Lipoprotein Levels (mg/dL) in Young Adultsa.
For a child identified with a lipid abnormality, three levels of care may be advisable: primary care, referral, and/or comanagement with a lipid specialist.
In general, healthy children with a family history of coronary artery disease and/or LDL-C values in the top quartile should be counseled and followed by their primary care provider.
Children with secondary causes of hyperlipidemia (e.g. diabetes, nephrotic syndrome) may be followed jointly by other subspecialists (e.g. pediatric endocrinologist, nephrologist) and usually do not require further evaluation by a specialist in dyslipidemia.
Children with heterozygous familial hypercholesterolemia (FH) can be managed jointly. The rare child with homozygous FH or another rare lipid disorder requires intensive therapy by a lipid specialist who works with dietitians specializing in the treatment of primary hyperlipidemia. The mainstays of therapy are diet and, for selected children, drug therapy.
Diet, although simple in concept, remains difficult to execute, requires a high level of motivation and cooperation from the family and child, and usually represents a considerable commitment in counseling. A professional dietitian is helpful but is a resource not usually available to a primary care provider.
Various diets have been advocated as interventions for children with primary hyperlipidemia, and they have common characteristics, most importantly the proportion of daily calories from fat (Table 12.4).
Table 12.4 Cardiovascular Health Integrated Lifestyle Diets (CHILD).
CHILD 1 (for children with elevated LDL-C)
|
CHILD 2-LDL (for children with elevated LDL-C additional risk factors or unresponsive to CHILD 1)
|
CHILD 2-TG (for children with elevated TG)
|
EER, estimated (daily) energy requirement.
Many characteristics are similar to the American Heart Association Step 1 and Step 2 Diets, and to the National Cholesterol Education Program (NCEP) Pediatric Panel diets.
Specifics of CHILD 1 and 2 diets, and detailed information regarding their indications and use, are available from National Heart, Lung, and Blood Institute (2012) The Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents. Full Report, NIH Publication No. 12-7486, National Institutes of Health, Bethesda, MD; www.nhlbi.nih.gov.
The Cardiovascular Health Integrated Lifestyle Diet (CHILD 1) is used for children whose LDL-C is borderline or high, with the goal of reducing LDL-C to the acceptable range.
As a next step, two different CHILD 2 diets can be used that are similar to the CHILD 1 diet, except that the levels of saturated fat and cholesterol are less, and for targeting of elevated triglycerides, replacement of simple sugars with complex carbohydrates (Table 12.4).
A detailed assessment by a trained specialist, such as a dietitian, is required; the diet must be carefully monitored to ensure adequate nutrient intake.
Drug therapy is inappropriate for most children with hyperlipidemia, as most respond to diet. When drugs are indicated, they are most effective in combination with diet therapy.
Other drugs commonly used in adults have had increasing use in children, usually in those with severe forms of hyperlipidemia. These drugs include fibrates, which lower TG (by accelerating enzymatic clearance of triglyceride-rich particles) and raise HDL, and ezetimibe, a molecular inhibitor of cholesterol absorption in the small bowel.
Nonpharmacologic treatments have included stem cell (bone marrow) transplantation for rare children with metabolic errors, such as homozygous FH.
Obesity
Mechanism of cardiovascular effect and definitions of obesity
Obesity is strongly associated with cardiovascular disease. It is multifactorial: 30% of cases are estimated to be genetic and 70% are from environmental factors that are modifiable. These factors may act through multiple interrelated mechanisms, including hyperlipidemia, hypertension, increased left ventricular mass, diabetes and insulin resistance, and obstructive sleep apnea (OSA), which may cause increased pulmonary resistance and right heart abnormalities.
Obesity is the presence of excess body fat, usually expressed as a proportion of total body mass. Like hyperlipidemia, the definition of obesity is somewhat arbitrary and depends on population “normals.” Although controversial, a commonly used definition of the term overweight in children is a proportion of body fat greater than the 85th percentile; the term obesity is reserved for those above the 95th percentile.
Comparing children in the 1990s with children studied in the 1960s, the number of “obese” children doubled.
Techniques for assessing obesity include indices of weight or mass compared with some reference, such as height, and also various measures of the proportion of body mass that is comprised of fat. Indices such as BMI, although rapid and simple to determine, do not reliably express adiposity, especially in children with lean body mass who are at the highest percentiles for age.
Various measures of the proportion of body mass consisting of fat can be determined. Varying with age and gender, it may be as much as 25% in normal infants. Measurements of triceps skin-fold thickness and bioelectric impedance are commonly used methods; they are more difficult to perform, require special equipment and/or training, and have limited reproducibility.
Clinical observation of a patient’s body fat and habitus is also important in interpreting measures of obesity.
Management
Management of overweight and obese children has become an important priority in preventive medicine because of the rising prevalence of obesity in developed societies. Effective intervention remains challenging, partly because of the difficulty in changing the strong societal factors that influence overweight and obesity in individual patients.
Although the definitions of overweight and obese are to some extent arbitrary, one should avoid classifying as obese any large-for-age child with high lean body mass who appears nonobese.
Rare hormonal and genetic causes (e.g. Klinefelter syndrome, hypothyroidism) should be ruled out. This can be done clinically, as most such affected children will be short (height ≤ 5th percentile) and have other physical clues to the diagnosis.
Increased physical activity rather than direct dietary intervention is the primary therapy for simple obesity. This is most effective when the patient has prescribed time for unstructured outdoor play, away from television and other sedentary pursuits. It may work by (1) increasing energy expenditure, (2) decreasing total caloric intake (presumably because the child is spending less time near food), and (3) altering the type of food ingested (e.g. lower percentage of fat calories) by an unknown mechanism.
Morbidly obese children or those who are refractory to simple management techniques benefit from an intensive team approach and require referral to a specialist in pediatric obesity.
Nutrition
Nutrition is an independent risk factor for cardiovascular disease through multiple mechanisms, most of which are interrelated to other risk factors, such as hyperlipidemia and obesity.
In general, the risk increases with a diet high in total calories, total fat, saturated fat, and salt and low in fiber, complex carbohydrates, antioxidants, and certain vitamins.
Commonsense guidelines for improving diet include eating a wide variety of foods, increasing the proportion of whole grains, fruits, and vegetables, and reducing overall fat intake, saturated fat, simple sugars, and salt.
Some specific nutrients have been associated with increased risk of cardiovascular disease, notably increased dietary consumption of trans-fatty acids. These fatty acids are chemically different to cis-fatty acids, leading to straighter and stiffer molecules when they are incorporated into cellular structures such as membranes.
Exercise
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


