Ischemic stroke cause remains undetermined in 30% of cases, leading to a diagnosis of cryptogenic stroke. Paroxysmal atrial fibrillation (AF) is a major cause of ischemic stroke but may go undetected with short periods of ECG monitoring. The Cryptogenic Stroke and Underlying Atrial Fibrillation trial (CRYSTAL AF) demonstrated that long-term electrocardiographic monitoring with insertable cardiac monitors (ICM) is superior to conventional follow-up in detecting AF in the population with cryptogenic stroke. We evaluated the sensitivity and negative predictive value (NPV) of various external monitoring techniques within a cryptogenic stroke cohort. Simulated intermittent monitoring strategies were compared to continuous rhythm monitoring in 168 ICM patients of the CRYSTAL AF trial. Short-term monitoring included a single 24-hour, 48-hour, and 7-day Holter and 21-day and 30-day event recorders. Periodic monitoring consisted of quarterly monitoring through 24-hour, 48-hour, and 7-day Holters and monthly 24-hour Holters. For a single monitoring period, the sensitivity for AF diagnosis was lowest with a 24-hour Holter (1.3%) and highest with a 30-day event recorder (22.8%). The NPV ranged from 82.3% to 85.6% for all single external monitoring strategies. Quarterly monitoring with 24-hour Holters had a sensitivity of 3.1%, whereas quarterly 7-day monitors increased the sensitivity to 20.8%. The NPVs for repetitive periodic monitoring strategies were similar at 82.6% to 85.3%. Long-term continuous monitoring was superior in detecting AF compared to all intermittent monitoring strategies evaluated (p <0.001). Long-term continuous electrocardiographic monitoring with ICMs is significantly more effective than any of the simulated intermittent monitoring strategies for identifying AF in patients with previous cryptogenic stroke.
Multiple studies have used a variety of cardiac monitors for atrial fibrillation (AF) detection after cryptogenic stroke and detection rates range from 0% to 25%. Differences in study design and absence of control groups have made interpretation of these results difficult and have limited the application of these studies in clinical practice. As a result, there are no firm recommendations on the duration of AF monitoring in a population with ischemic stroke beyond 24 hours. The Cryptogenic Stroke and Underlying Atrial Fibrillation trial (CRYSTAL AF) compared the rate of AF detection in patients with cryptogenic stroke randomly assigned to either conventional follow-up (control) or continuous monitoring with an insertable cardiac monitor (ICM, Reveal XT; Medtronic, Minneapolis, Minnesota). At 6, 12, and 36 months, the rates of AF detection were 8.9%, 12.4%, and 30% in the continuous monitoring arm versus 1.4%, 2.0%, and 3.0% in the control arm, respectively (p <0.001 for all). Given the invasive nature and cost associated with device insertion, the question remains whether currently available forms of external monitoring can substitute for the long-term continuous monitoring afforded by an ICM. The purpose of this analysis was to assess the sensitivity and negative predictive value (NPV) of various simulated durations and periodicities of external monitoring strategies for AF detection in a population with cryptogenic stroke.
Methods
The design of the CRYSTAL AF study has been previously published. Briefly, patients aged >40 years who presented with a cryptogenic stroke or transient ischemic attack (TIA) within 90 days were included. They were randomized within 14 days to conventional follow-up or ICM. Patients with history of AF or atrial flutter were excluded. Patients were also excluded if there was a permanent indication or contraindication to anticoagulation or if they needed or had a pacemaker or implantable cardioverter defibrillator. Device data from days 1 to 345 after insertion were evaluated for the purposes of this analysis.
In the CRYSTAL AF study, AF was defined as an episode of irregular heart rhythm without detectable p-waves lasting >30 seconds in duration. AF episodes were independently adjudicated. In this analysis, we simulated several intermittent monitoring strategies and compared them to continuous rhythm monitoring with an ICM in the intervention arm of the CRYSTAL AF trial. These intermittent monitoring strategies, including both single short-term and repetitive periodic monitoring, are depicted in Figure 1 . Short-term monitoring included 24-hour Holter monitor, 48-hour Holter monitor, 7-day Holter monitor, 21-day event recorder, and 30-day event recorder. Periodic monitoring consisted of quarterly monitoring through 24-hour Holter, 48-hour Holter, and 7-day Holter and monthly 24-hour Holters.
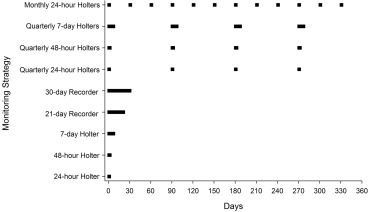
The initial day for each intermittent monitoring strategy simulation was randomly selected from a uniform distribution among days 1 to 14 after ICM placement. For example, to simulate a 7-day Holter monitor, we evaluated whether the ICM detected AF on any of 7 consecutive days beginning randomly on days 1 to 14 after device insertion. For monitoring strategies involving repetitive periodic monitoring, all subsequent monitoring periods were based on a fixed number of days from the randomly selected initial day of monitoring. For example, quarterly 24-hour Holter monitoring was simulated by evaluating whether the ICM detected AF on a randomly selected day within the first 14 days after device insertion or on days 90, 180, and 270 from that initially selected day. A minimum follow-up duration of 345 days was required of all patients to allow for simulation of the longest monitoring scenario (12 monthly 24-hour Holters) with the latest randomly selected monitoring start day (day 14). All simulations were repeated 10,000 times, and the mean value of these simulations are reported.
From these simulations, the patient-level sensitivity and NPV were estimated through comparison with actual AF events recorded by the ICM as the “gold standard.” Sensitivity measures the proportion of patients with AF detected by the ICM who would have been identified as having AF through intermittent monitoring. NPV measures the proportion of patients without AF detected through intermittent monitoring who were correctly identified as being free from AF through the ICM.
Continuous variables are reported as means with standard deviations, and categorical variables are reported as frequency counts with percentages. The McNemar test was used to compare the proportions of patients with AF detected through intermittent monitoring strategies versus continuous monitoring. SAS version 9.2 (SAS Institute Inc., Cary, North Carolina) was used for all statistical analyses. A significance level of 0.05 was used for all statistical tests.
Results
Of the 221 patients who were randomized to the ICM arm in the CRYSTAL AF trial, 26 patients had their devices inserted more than 14 days after randomization and an additional 27 patients did not have data available for analysis from days 1 to 345 after insertion. Consequently, 168 patients form the basis of this analysis ( Figure 2 ). Baseline characteristics are provided in Table 1 . There were 30 patients (18%) who were found to have AF with continuous monitoring within the initial 345 days. The median AF burden was 0.0336 hours/day (interquartile range [IQR] 0.0114 to 0.1033), and the median percent days with AF was 5.5% (IQR 2.9 to 18.0). Their median AF duration on the single day with maximal burden was 3.9 hours (IQR 0.1 to 13.0 hours). Of the 30 patients with AF detected by the ICM, 23 patients (77%) had a maximum 1-day AF burden greater than 6 minutes.
| Variable | |
|---|---|
| Age (years) | 61.3 ± 11.0 |
| Men | 115 (68%) |
| Index Event – Stroke | 150 (89%) |
| Index Event – Transient Ischemic Attack | 18 (11%) |
| CHADS 2 Score (mean) | 2.9 ± 0.8 |
| 2 | 54 (32%) |
| 3 | 75 (45%) |
| 4 | 35 (21%) |
| 5 | 3 (2%) |
| 6 | 1 (1%) |
| Heart Failure | 5 (3%) |
| Hypertension | 106 (63%) |
| Diabetes Mellitus | 22 (13%) |
Figure 3 depicts the sensitivity and NPV of one-time short-term external monitoring for AF detection. The sensitivity, compared to the ICM, was lowest for a single 24-hour Holter (1.3%) and highest for a 30-day monitor (22.8%), whereas the NPV ranged from 82.3% to 85.6%. The results of repetitive periodic monitoring ( Figure 3 ) are also limited with 4 quarterly 24-hour Holters demonstrating a sensitivity of 3.1% and 4 quarterly 7-day Holters showing the greatest sensitivity at 20.8%. The NPV for repetitive monitoring was 82.6% to 85.3%, similar to the one-time monitoring strategies. For all the intermittent monitoring strategies explored in this analysis, both the sensitivity and NPV were significantly lower than that of continuous arrhythmia monitoring (p <0.001).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


