INTRACARDIAC ECHOCARDIOGRAPHY TO GUIDED Transseptal PUNCTURE
CONOR D. BARRETT, LUIGI DI BIASE, J. DAVID BURKHARDT, RODNEY P. HORTON, SHELDON M. SINGH, MOUSSA MANSOUR, ANDREA NATALE
For many interventionalists who are training in left atrial mapping and ablation, gaining access to the left atrium (LA) is perceived as a stressful and challenging portion of the procedure. In expert hands, transseptal punctures can be safely performed with the utilization of fluoroscopy alone, but there are many instances where the additional information obtained by intracardiac echocardiography (ICE) is invaluable.1,2 This is more so when patients are therapeutically anticoagu-lated for the procedure, when the inherent risks are higher. To reduce the periprocedural risk of stroke and access complications, many centers now routinely perform atrial fibrillation (AF) ablation procedures while the patient is therapeutically anticoagulated with warfarin and administer heparin prior to the transseptal puncture.3-5
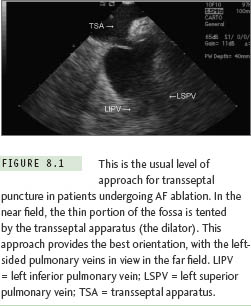
Although for some procedures (eg, mapping of accessory pathways), a retrograde aortic approach may be undertaken, this obviously requires arterial access and increases the risk of access complications. A transseptal approach frequently is easier and necessary for left-sided pathway ablations, and is obligatory in some patients (eg, those with severe aortic stenosis or with an artificial aortic valve). For other procedures, in particular ablation for AF, transseptal catheterization is obligatory.6 The usual location of transseptal puncture for AF ablation procedures is shown in Figure 8.1.
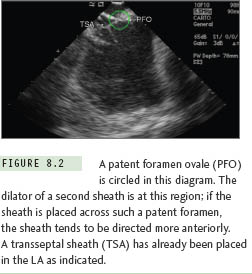
Because of the inherent risks associated with transseptal puncture, it makes sense that all necessary precautions are undertaken to ensure the safety of the procedure. In an analogous situation, it has been previously observed that central venous access complications (including the reduction of attempts for success) can be reduced by direct, real-time visualization with ultrasound.7 Moreover, as those familiar with AF ablation will testify, the appropriate approach to the transseptal and subsequent orientation of the sheaths in the left atrium is of extreme importance in increasing the ease of mapping and ablation of the posterior wall and the pulmonary venous antra. If a patent foramen ovale exists, passage through it is possible; such a course directs the transseptal apparatus in a more anterior direction, which is a suboptimal orientation for AF ablation procedures. The appearance of a second transseptal dilator at the level of a patent foramen ovale (PFO) is shown in Figure 8.2. It therefore makes sense to employ a real-time imaging modality that will increase the safety of transseptal puncture and, through correct orientation, decrease subsequent procedural time. Intracardiac echocardiography (ICE) is such a modality.
Procedural Considerations
Two forms of intracardiac echocardiography transducers are available: (1) a rotational (radial/mechanical) crystal transducer providing a circumferential view of the area of interest and (2) a phased array transducer providing sector visualization of the area of interest. Both catheters are available with imaging frequencies between 5 MHz to 10 MHz. The rotational catheters provide good quality near-field images and are employed in coronary interventions most frequently. It is our practice to utilize a phased-array catheter (available in 8 F and 10 F diameters), as these catheters provide better real-time definition of the anatomy in both the near- and far-field perspectives.
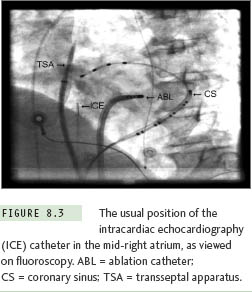
Transseptal punctures are routinely performed via right femoral venous access. The ICE catheter is advanced from the left femoral vein. It is advisable to advance the catheter into the inferior vena cava (IVC) under fluoroscopic guidance, which can be achieved by gentle flexion of the catheter at the level of the iliac vein. The catheter is then advanced into the right atrium. It is our general practice to position the ICE catheter in the mid-right atrium for the purpose of transseptal puncture (Figure 8.3). Gentle clockwise rotation of the ICE catheter moves the plane of imaging posteriorly, such that the anterior (aortic root) and subsequently more posterior structures (anterior left atrium, mitral valve, and left atrial appendage) are sequentially viewed (Figures 8.4, 8.5). Further clockwise rotation of the catheter moves the plane of imaging more posteriorly, such that the left-sided pulmonary veins come into view in the far field (Figure 8.6). At this orientation, in the near field, the interatrial septum (IAS) is clearly visualized. On occasion, if the ICE catheter is located too close to the septum, gentle retroflexion of the catheter provides for better imaging of the IAS. Further clockwise rotation brings the right-sided pulmonary veins into the field of view. The IAS remains in view in the near field throughout such posterior rotation. It is easily seen that the more posterior the orientation, the shorter the distance from the IAS to the opposing LA wall and roof (Figure 8.7). A puncture at this site, particularly without ICE guidance, may result in cardiac perforation and tamponade. Transseptal puncture should not be attempted in the more anterior plane with the aortic valve in view; an attempt at left atrial access at this level may result in damage or perforation of the aortic root.
The basic methodology employed for the transseptal puncture is the same as when utilizing fluoroscopy alone. A long 0.032-inch guidewire is advance to the superior vena cava (SVC) under fluoroscopic guidance. It is good practice to visualize the J tip of the guidewire outside the heart (to at least the level of the tracheal carina) to ensure that the long sheath is not inadvertently placed in the right atrial appendage. The long transseptal sheath of choice is advanced over the long J wire. The guidewire is removed, and the dilator aspirated and flushed with heparinized saline. Next, a flushed transseptal needle is advanced (with its stylet in place) to within 2 cm to 4 cm of the tip of the dilator. The stylet is withdrawn, and the needle is again aspirated and flushed with heparinized saline and then with radiopaque contrast. The whole apparatus is gently withdrawn into the right atrium in the left anterior oblique (LAO) view, with the guiding orientation (marker on the transseptal needle) usually oriented at between 4 o’clock and 6 o’clock so as to avoid the aortic root. A “jump” to the septum is usually clearly visualized on fluoroscopy, and the exact positioning of the tip of the apparatus is then confirmed on the ICE image (Figure 8.1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


