FETAL ARRHYTHMIAS
Introduction
The first organized fetal heartbeats are seen very early in pregnancy, during the formation of the primitive heart tube, at around 12 days of gestation. Thereafter, the conduction system continues to develop and it becomes functionally mature at around 16 weeks of gestation.1 Based on the fetal activity and the gestational age, the fetal heart rate changes with a little beat-to-beat variation throughout the pregnancy. It ranges between 110 and 180 beats per minute (bpm) during the first trimester with a maximum heart rate at around 9 weeks of gestation.2 After the first trimester, fetal heart rate decreases to the range of 110 to 150 bpm with an average rate of 135 bpm at near term.3
Fetal arrhythmias are not uncommon and seen in approximately 1% to 3% of all pregnancies.4 Approximately 90% of these are transient, and most of them occur as atrial ectopic beats that are usually benign and do not result in any significant hemodynamic compromise. On the other hand, some of these arrhythmias result in adverse hemodynamic state and are associated with poor prognosis (ie, ventricular fibrillation [VF]) while some others may be associated with major congenital anomalies (ie, complete heart block) and may result in intrauterine demise. Therefore, diagnosis of fetal arrhythmias and their in utero management are of utmost importance. In this chapter, the fetal arrhythmias and their management options are reviewed.
Diagnosis of Fetal Arrhythmias
Diagnosis of fetal arrhythmias in utero may be very challenging. The main diagnostic tool is fetal echocardiogram. More specifically, M-mode and pulsed-wave Doppler echocardiogram are used to investigate fetal heart rate and timing of the atrial and ventricular mechanical events.
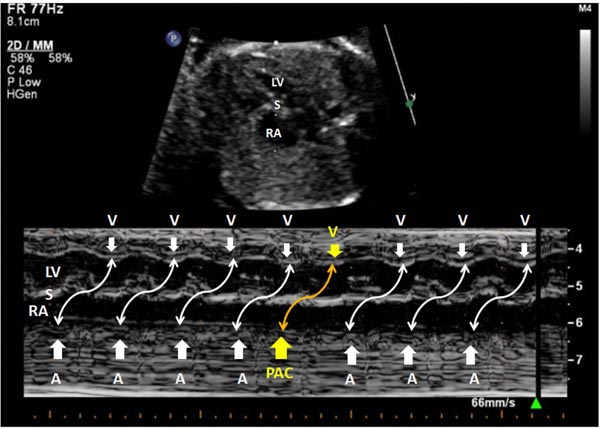
The M-mode recordings are taken from atrial and ventricular tissues simultaneously.5 Both the atrial and ventricular rates as well as the relation between atrial and ventricular contractions can be assessed from the M-mode recordings (Figure 6.1). However, this technique has limitations to define the onset and the peak of atrial and ventricular contractions, and therefore may not be useful to measure the atrioventricular (AV) time intervals accurately.6
Figure 6.1. M-mode recording in a fetus with a normal sinus rhythm. The cursor intersects the RA, S and LV; RA, right atrium; S, ventricular septum; LV, left ventricle; A, atrial contractions; V, ventricular contractions.
The pulsed-wave Doppler recordings are taken by placing the pulsed Doppler gate across the mitral and aortic valve, or pulmonary artery (PA) and pulmonary veins, or renal artery and renal vein, as well as superior vena cava (SVC) and aorta (Ao).6 With this technique, simultaneous signals from atrial and ventricular contractions can be obtained, and, in addition to atrial and ventricular rate, various time intervals including AV interval (PR interval) can be measured (Figure 6.2).
Figure 6.2. Pulsed-wave Doppler recording in a fetus with a normal sinus rhythm. The Doppler gate is placed at left ventricular (LV) inflow (mitral valve) and LV outflow (aortic valve). The time interval between the beginning of the A wave and the beginning of the V wave identifies the AV interval or mechanical PR interval, which is similar to the electrical PR interval seen on surface ECG albeit somewhat longer than the electrical PR interval, because the AV interval also includes the isovolumic ventricular contraction phase. In this fetus, the AV interval measures 116 ms. The normal AV interval in a fetus (from the mitral/aortic valves region) is 0.12 ± 0.02 second. LV, left ventricle; A, atrial contractions; V, ventricular contractions; E, early filling Doppler wave of left ventricular inflow (mitral valve); AV, atrioventricular.
Tissue Doppler imaging is another echocardiographic technique and can also be used for assessment of fetal heart rhythm. With this technique, fetal cardiac segmental wall motion and timing of atrial and ventricular systolic movements can be analyzed. In addition, cardiac intervals and myocardial velocities can be measured.7
Other diagnostic tools for fetal arrhythmias are fetal ECG and magnetocardiography. These are available only in few referral centers and mostly used for research purposes, and therefore are beyond the scope of this presentation.
Fetal Arrhythmias and Their Management
Fetal arrhythmias may be classified into 3 main groups and further subgroups as summarized in Table 6.1.
Table 6.1. Classification of fetal arrhythmias
| I. Irregular fetal heart rhythm |
a. Premature atrial contractions (PACs) b. Premature ventricular contractions (PVCs) |
| II. Fetal bradyarrhythmias |
|
| III. Fetal tachyarrhythmias |
|
Irregular Fetal Heart Rhythm
This group of abnormal fetal rhythm is the most common fetal arrhythmia and the main reason for referral for evaluation. The irregular rhythm can be secondary to premature atrial contractions (PACs) as seen in most of the cases and rarely secondary to premature ventricular contractions (PVCs).
PACs PACs are usually benign. The premature beats can be conducted or blocked in which case a short pause following the premature beat will be seen (Figures 6.3–6.5). They are most commonly seen in the late second trimester and near term during the pregnancy. Approximately 1% to 2% of PACs are seen in cases with congenital heart diseases.8 Around 2% to 3% of the cases with PACs may have in utero or neonatal progression to sustained tachycardia, which can occur especially in cases with slow ventricular rate secondary to multiple blocked PACs in bigeminy or trigeminy (Figure 6.6).6,8–10 When there is impaired cardiac function in association with PACs, there is a high suspicion for supraventricular tachycardia (SVT) and these cases should be monitored closely until PACs resolve or until delivery.
Figure 6.3. M-mode recording in a fetus with PACs. The cursor intersects the R, S, and LV. The fifth labeled atrial contraction (PAC) occurred earlier, and it is followed with a ventricular contraction indicating the PAC is conducted. The relations between atrial and ventricular contractions are shown with a curved double-arrow connector for each beat with the yellow connector showing PAC and the ventricular contraction after its conduction. LV, left ventricle; S, ventricular septum; RA, right atrium; A, atrial contractions; V, ventricular contractions; PAC, premature atrial contraction.
Figure 6.4. Pulsed-wave Doppler recording from the LV inflow and LV outflow in a fetus with PACs. An isolated PAC occurred sooner, and the inflow Doppler waveform showed only an A wave since it occurred earlier and fused with the E wave. There is a ventricular contraction following this PAC, indicating the PAC is conducted. The view in the left upper corner of the image shows the cardiac chambers and the position of the Doppler cursor and gate in detail. LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle; A, atrial contractions; V, ventricular contractions; PAC, premature atrial contraction.
Figure 6.5. Pulsed-wave Doppler recording from the right ventricular inflow (tricuspid valve) in a fetus with PACs. The PACs are seen in a bigeminy pattern (occurring in every other beat). The Doppler wave pattern of PACs show only A wave without preceding E wave because they are fused. PAC, premature atrial contraction; A, atrial contractions; E, early filling Doppler wave from right ventricular inflow.
Figure 6.6. Pulsed-wave Doppler recording from umbilical artery in a fetus with blocked PACs in bigeminy and trigeminy patterns. The waveforms resulting from the PACs are shown with yellow arrow. The first, second, and fourth PACs are in trigeminy pattern whereas the third PAC is in bigeminy pattern.
PVCs PVCs are also benign in most of the cases and are rarely seen. However, PVCs may be associated with myocarditis and long QT syndrome; therefore, these cases should be monitored with serial echocardiographic evaluation. In cases with difficulty differentiating the PVCs from the PACs, the presence of tricuspid regurgitation or smaller A wave in pulsed-wave Doppler interrogation of the inferior vena cava helps to identify these beats as PVCs.
Management Most of these irregular fetal heart rhythms are benign, do not result in any hemodynamic compromise, and resolve spontaneously and therefore do not require any treatment or intervention. The fetuses with irregular heart rhythm should be monitored closely (weekly or biweekly) to evaluate the fetal heart rate and rhythm. In addition, the mother should be counseled to avoid the triggering factors such as smoking, excessive caffeine consumption, and medications that have stimulant effects on the heart (ie, beta-mimetics).
Fetal Bradyarrhythmias
Fetal bradyarrhythmias are characterized by slow heart rate less than 100 bpm. This abnormal rhythm may be transient or sustained (persistent).
Benign transient fetal bradycardia This type of bradyarrhythmia occurs as a transient decrease in fetal heart rate for a brief of period time (less than 1–2 minutes). These are usually benign and do not cause any adverse hemodynamic effects. It often can be seen with increase in vagal stimulation (ie, increase in abdominal pressure during fetal echocardiographic examination if the probe is used with high pressure).
Sinus bradycardia Sustained fetal sinus bradycardia is rarely seen and may result from fetal distress with acidemia, congenital long QT syndrome, and sinus node dysfunction. It may also be seen in fetuses with heterotaxy syndromes with left atrial isomerism where the sinus node may be congenitally absent.11,12
Fetal sinus bradycardia is characterized with slow atrial rate (less than 100 bpm) with normal 1:1 AV conduction.
In cases with a family history positive for a long QT syndrome and/or in cases with intermittent episodes of ventricular tachycardia (VT) with 2:1 AV conduction (2:1 AV block), congenital long QT syndrome should be suspected.11,13
Blocked PACs in bigeminy or trigeminy These types of fetal bradyarrhythmias are usually benign and resolve with increase in fetal activity. The atrial rate is higher than the ventricular rate; thus, these arrhythmias should be differentiated from AV heart block, which also presents with a faster atrial rate compared with the ventricular rate. Assessment of the time intervals between consecutive atrial impulses is helpful for the differentiation. The time intervals between consecutive atrial beats will be relatively constant in AV heart block, whereas it will be shortened on every second beat in bigeminy with blocked PACs and on every third beat in trigeminy with blocked PACs. When the blocked PACs are very frequent, there may be hemodynamic changes; Figure 6.6 shows a pulsed-wave Doppler waveform of the umbilical artery in a fetus with frequent blocked PACs.
Congenital AV blocks (AV heart blocks)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree