Wide-Complex Tachycardia: Ventricular Tachycardia versus Supraventricular Tachycardia
Wide-complex tachycardia (WCT) is defined as a tachyarrhythmia with a rate >100 beats/min (bpm) and a QRS duration >120 milliseconds on a 12-lead electrocardiogram (ECG). Utilizing the ECG, the correct mechanistic diagnosis of a WCT rhythm is often difficult. Besides being an intellectual exercise, it is very important to establish the correct diagnosis in order to deliver appropriate acute therapy and to plan subsequent long-term patient management. Several criteria and algorithms have been developed to help distinguish among different causes of WCT. When used individually, none of these criteria reaches 100% specificity; however, when properly applied together and in conjunction with the clinical history and presentation, the algorithms serve as a guide to the correct diagnosis in the majority of the cases.
WCT can result from either a ventricular or a supraventricular mechanism. Ventricular tachycardia (VT) originates below the level of the His bundle. Supraventricular tachycardia (SVT) originates in or involves structures above the His bundle. SVT may involve atrial tachycardia, atrial fibrillation, atrial flutter, atrioventricular (AV) node reentrant tachycardia (Fig. 30.1), or AV reentrant tachycardia. AV reentrant tachycardia may be either orthodromic reentrant tachycardia or antidromic reentrant tachycardia (Fig. 30.2). Orthodromic reentrant tachycardia occurs when antegrade ventricular conduction occurs via the AV node and retrograde conduction to the atrium is via the accessory pathway. Antidromic reentrant tachycardia occurs when ventricular antegrade conduction occurs over the accessory pathway and retrograde conduction occurs via the AV node.
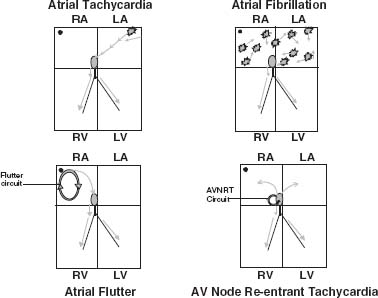
FIGURE 30.1 Supraventricular tachycardia.
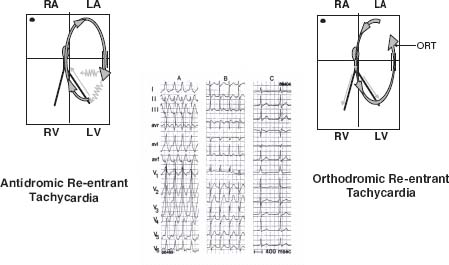
FIGURE 30.2 AV reentrant tachycardia.
DIFFERENTIAL DIAGNOSIS
WCT can occur by three different mechanisms:
1. VT is the most common cause of WCT in the general population, accounting for >80% of all cases. It is even more common in patients with structural heart disease, and it may occur in 98% of patients with a prior history of a myocardial infarction. VT may be either monomorphic or polymorphic. Monomorphic VT occurs when the QRS morphology is stable and uniform, whereas polymorphic VT occurs when the QRS complexes vary in morphology.
2. The second mechanism of WCT occurs when the tachycardia originates above the ventricle and has abnormal ventricular activation, also known as SVT with aberrancy. It accounts for 15% to 20% of all cases of WCT and includes a variety of disorders.
a. The first example is SVT with bundle branch block aberration, which may be either a right bundle branch block (RBBB) or a left bundle branch block (LBBB) morphology (Fig. 30.3). Activation of the ventricle through the His–Purkinje system (His bundle and both bundle branches) results in a narrow QRS complex. Activation of the ventricle unilaterally via one bundle branch results in a wide QRS complex, because activation of the remainder of the ventricular myocardium is dependent on slow myocardial conduction. Aberration occurs when there are abnormalities of intraventricular conduction in response to changing heart rate, and when the conduction over the His–Purkinje conduction system is delayed or blocked in either the right or left bundle branch. RBBB is more common, occurring in 80% of cases. The aberration may be fixed, occurring in normal sinus rhythm at a slow heart rate, or it may be functional and present only during tachycardia.
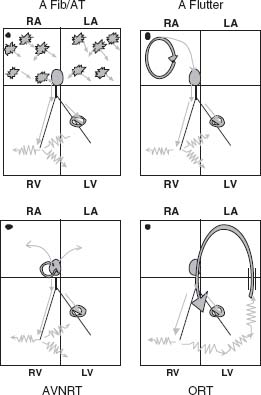
FIGURE 30.3 SVT with bundle branch block.
b. SVT with antegrade conduction via an accessory pathway, such as in Wolff–Parkinson–White syndrome, accounts for 1% to 5% of all WCT. The accessory pathway is an anomalous AV connection that inserts directly into ventricular myocardium at the base of the ventricle along the mitral or tricuspid valve annulus. Ventricular activation is initiated at this insertion point and is termed ventricular pre-excitation. Pre-excited tachycardia can occur with SVT with antegrade conduction via the accessory pathway. The accessory pathway is not part of the tachycardia circuit and is not essential for its perpetuation. The other form of pre-excited tachycardia can occur with antidromic reciprocating tachycardia, in which the accessory pathway is part of the tachycardia circuit (Fig. 30.4).
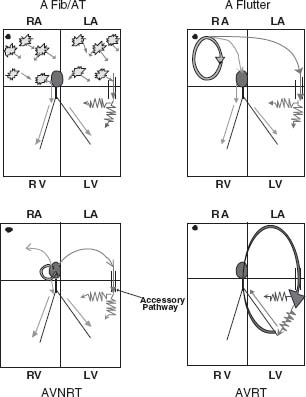
FIGURE 30.4 SVT with pre-excitation.
c. Another form of WCT is SVT with an intraventricular conduction delay. This can occur in patients with cardiomyopathy, corrected congenital heart disease such as tetralogy of Fallot, or Ebstein anomaly, in which myocardial conduction is further impaired. The conduction abnormality is usually apparent during normal sinus rhythm.
d. Some medications are capable of producing nonspecific widening of the QRS complex during SVT. These include Na+ channel blockers, especially Class IC agents (flecainide, encainide), less so Class IA antiarrhythmics (quinidine, procainamide, disopyramide), and amiodarone. The most common example is a patient with atrial flutter being treated with flecainide. Flecainide can induce flutter rate slowing to permit 1:1 AV nodal conduction and a secondary increase in the ventricular rate with a wide QRS complex. This is as a result of the slow ventricular conduction in response to the Na+channel blockade. This can be easily and erroneously interpreted as VT (Fig. 30.5).
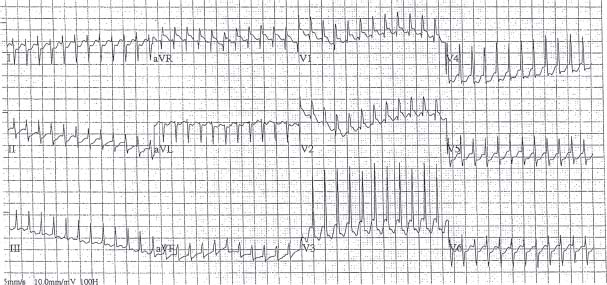
FIGURE 30.5 Atrial Flutter with 1:1 conduction.
e. Electrolyte abnormalities such as hyperkalemia can cause widening of the QRS complex and can be mistakenly interpreted as VT. The morphology is typically LBBB.
3. Ventricular paced rhythms can also mimic WCT (Fig. 30.6). Most pacemakers are dual chamber, with a lead in the right atrium and one in the right ventricle. Pacing of the right ventricle causes an LBBB QRS morphology. The surface ECG representation of the pacing stimulus is less apparent with the use of bipolar pacing modes and a resultant decrease in the energy requirement for reliable ventricular pacing. Therefore the pacing spike may be overlooked or even absent from ECG tracings. A wide QRS tachycardia can occur in any SVT with atrial tracking, in which the ventricle is paced in response to atrial sensing. In these cases, it is essential to obtain an adequate history and to analyze a previous ECG to evaluate the baseline morphology of the QRS complex.
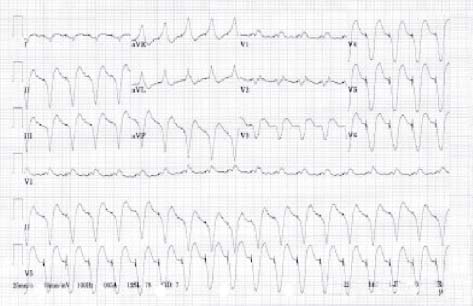
FIGURE 30.6 Ventricular paced tachycardia.
4. Pacemaker-mediated tachycardia can also produce a WCT. The pacemaker is itself responsible for the tachycardia when ventricular pacing results in retrograde conduction to the atrium. The pacemaker senses the atrial conduction, resulting in ventricular pacing, which in turn is followed by retrograde conduction to the atrium, resulting in “endless loop tachycardia” (Fig. 30.7).
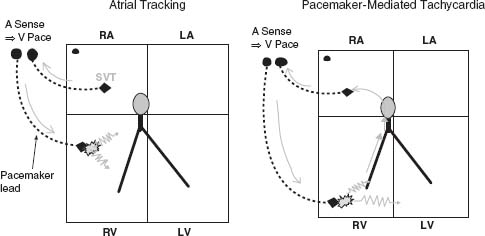
FIGURE 30.7 Ventricular paced tachycardia. Left: Atrial tracking. Right: Pacemaker-mediated tachycardia.
5. Lastly, artifacts from recording equipment problems (such as fast-sweep speed recording) or from external repetitive motion (such as brushing teeth) can present as “WCT” (Fig. 30.8).
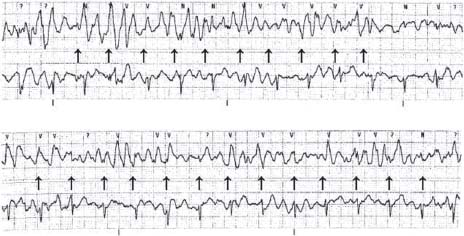
FIGURE 30.8 Artifact mimicking WCT.
DIAGNOSIS
Clinical Presentation
In order to diagnose the etiology of the WCT, it is important to evaluate the clinical presentation. As mentioned before, obtaining an accurate patient history is crucial in formulating an accurate rhythm diagnosis. A prior history of heart disease, myocardial infarction, or congestive heart failure makes the diagnosis of VT highly suggestive as the cause of the WCT. Akhtar et al. have reported that the positive predictive value of a WCT representing VT in a patient with a prior history of myocardial infarction is 98%. Tchou reported that of patients who had a prior myocardial infarction and a first episode of tachycardia occurring after the infarction, 28 of 29 patients presented with VT and were diagnosed correctly. The older the patient is, the more likely that the tachycardia is ventricular; however there is a significant overlap with SVT patients. It is also helpful to know if there is any presence of congenital heart disease, or if the patient has a pacemaker or defibrillator. Knowing that the patient has an implantable cardioverter-defibrillator (ICD) raises a concern for pacemaker-associated tachycardia, but more important, the presence of the device suggests that the patient has risk factors for VT. A history of a prior similar episode may also be useful. The first occurrence of the arrhythmia after a myocardial infarction is highly suggestive of VT, whereas SVT may be more likely if there is recurrence of the arrhythmia over several years. The presence of other medical conditions can point to a diagnosis of WCT. For example, in a patient with renal failure, the WCT may be attributable to hyperkalemia. In a patient with known peripheral vascular disease, the WCT may be indicative of VT, because such patients are likely to have underlying coronary artery disease.
Knowing what medications the patient is taking, especially cardiac medications, is vital when evaluating WCT. It is important to identify medications that prolong the QT interval, such as dofetilide, sotalol, quinidine, and erythromycin, which can all cause torsade de pointes, a form of polymorphic VT. Electrolyte abnormalities caused by certain medications such as diuretics (hypokalemia and hypomagnesemia) or angiotensin-converting enzyme (ACE) inhibitors (hyperkalemia) may predispose to VT. Patients who are on digoxin are more susceptible to an arrhythmia when hypokalemia is present. The most common arrhythmias are monomorphic VT, bidirectional tachycardia, and junctional tachycardia, and typically occur when the plasma digoxin concentration is >2.0 ng/mL. As stated earlier, Class IC agents can cause rate-related aberrant conduction during SVT. Symptoms such as palpitations, lightheadedness, or chest pain are generally not useful in evaluating the etiology of the WCT.
One of the priorities in evaluating a patient with WCT is determining if the patient is hemodynamically stable or unstable. This requires knowing the patient’s blood pressure and heart rate. In a patient who is unstable, emergency cardioversion is required and the mechanism of the arrhythmia may not necessarily be known. VT can be present when the patient is hemodynamically stable and should not be mistaken for SVT, lest the patient be given inappropriate medical therapy (such as adenosine or verapamil) that can lead to hemodynamic compromise with VT. When the patient is hemodynamically stable, a more detailed physical exam can be performed. Inspection of the chest can point to underlying cardiovascular disease when there is a sternal incision, a pacemaker, or defibrillator.
AV dissociation occurs in 60% to 75% of patients with VT and is a result of the atria and ventricles depolarizing independently. It almost never occurs in SVT. This finding is usually identifiable on the surface ECG. However, it is also possible to make this diagnosis on physical exam by assessing the jugular venous pulsation. Cannon A waves are irregular pulsations that are of greater amplitude than the normal jugular venous waves, and occur intermittently when the atrium and ventricle contract simultaneously. When the tachycardia rate is slower, there can be variable intensity of the first heart sound. However, evaluating this may not be practical in an acute situation.
Laboratory tests should be performed for patients with WCT to determine potassium and magnesium levels. If the patient is on digoxin, it is also important to obtain the serum digoxin level. If a chest x-ray is available, one can readily identify the presence of a pacemaker, defibrillator, or sternal wires that might point to underlying structural heart disease.
Provocative Maneuvers
Certain bedside maneuvers can be performed to distinguish VT from SVT. The Valsalva maneuver or carotid sinus massage enhances vagal tone, which depresses sinus nodal and AV nodal activity. These maneuvers will slow the heart rate during sinus tachycardia, but once they are completed, the heart rate will increase again. If the patient is in SVT, these maneuvers may terminate the rhythm. If the patient is in an atrial tachycardia or flutter, the rhythm will persist though the ventricular rate may be slower, thus uncovering the background atrial activity. These maneuvers can also elicit VA conduction block, which can induce AV dissociation during VT.
Certain medications can be used to diagnose the tachyarrhythmias. For example, adenosine, given in 6- to 12-mg boluses intravenously during WCT, can result in one of the following scenarios:
1. The tachycardia terminates, making it more likely to be supraventricular in etiology, invoking AV node participation. Some atrial tachycardias may also terminate with adenosine.
2. AV block occurs, uncovering the background atrial activity such as atrial tachycardia, flutter, or fibrillation, thus allowing the diagnosis of an atrial tachyarrhythmia.
3. If 1:1 AV association is present and evident during WCT, adenosine-induced AV block results in AV dissociation, thus making the diagnosis VT



