CHAPTER 1 What is echo?
1.1 BASIC NOTIONS
Ultrasound production and detection
The wavelength of sound equals the ratio of velocity to frequency. In heart tissue, ultrasound with a frequency of 5 MHz has a wavelength of about 0.3 mm. The shorter the wavelength, the higher the resolution. As a rough estimate, the smallest size that can be resolved by a sound is equal to its wavelength. On the other hand, the smaller the wavelength of the sound, the less its penetration power. So a compromise has to be struck between resolution and penetration. A higher frequency of ultrasound can be used in children since less depth of penetration is needed.
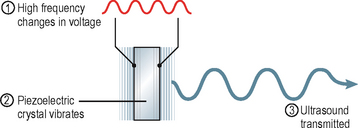
Ultrasound results from the property of certain crystals to transform electrical oscillations (varying voltages) into mechanical oscillations (sound). This is called the piezoelectric effect (Fig. 1.1). The same crystals can also act as ultrasound receivers since they can effect the transformation in the opposite direction (mechanical to electrical).
Two quantities are measured in an echo:
1.2 VIEWING THE HEART
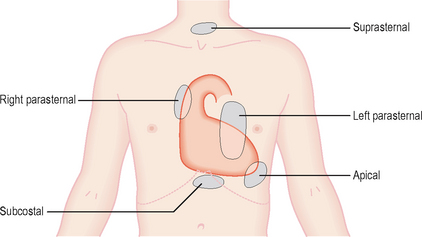
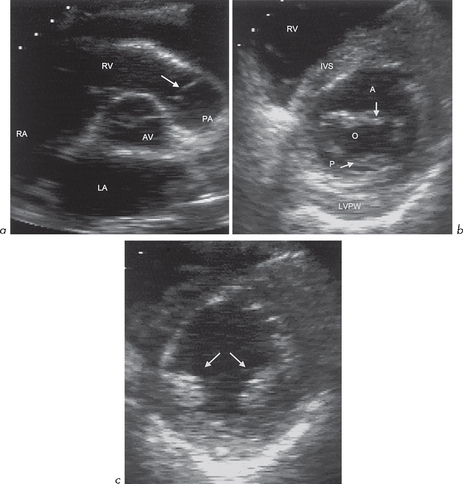
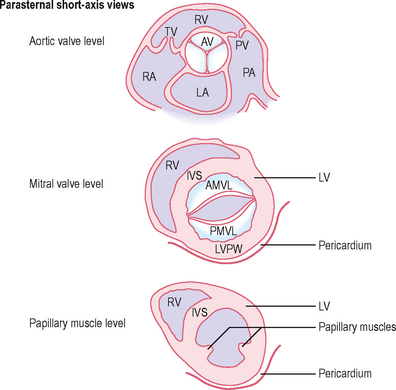
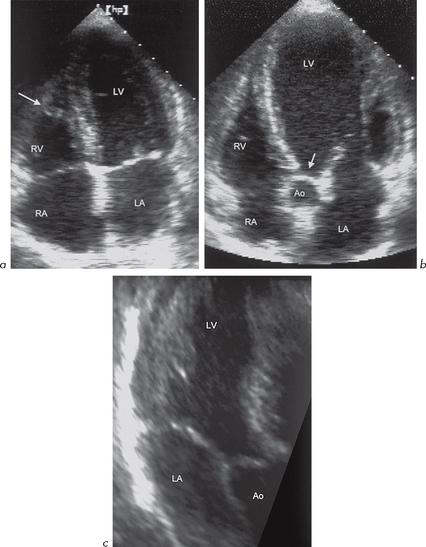
Echo ‘windows’ and views (Fig. 1.2)
Rarely, an echo study is impossible.
Left parasternal window.
(2nd–4th intercostal space, left sternal edge):
Apical window.