Visceral Aortic Endarterectomy
Timur P. Sarac
Revascularization for mesenteric ischemia is necessary when patients present with symptoms of mesenteric angina. Additionally, they may have chronic bowel dysfunction, which can be either diarrhea and/or constipation. The decision to proceed with revascularization through open surgical operations should be made after careful consideration of minimally invasive endovascular options. When open surgery is contemplated, the operative approach is surgeon dependent. In doing so one takes into account that in most circumstances, celiac, superior mesenteric (SMA), and inferior mesenteric artery (IMA) occlusive disease involves the orifice and is a continuation of aortic disease (Fig. 11.1). The options for revascularization include percutaneous angioplasty and stent, open bypass surgery, and transaortic visceral endarterectomy. In certain situations visceral aortic endarterectomy may be preferred and have specific indications. These scenarios include:
Focal atherosclerosis involving the orifice of the celiac and SMA. We do not typically include the IMA, as doing so is more extensive and rarely necessary.
Coral reef plaque causing obstructive of both the aorta and mesenteric artery flow.
Failed attempt at endovascular therapy with significant aortic disease.
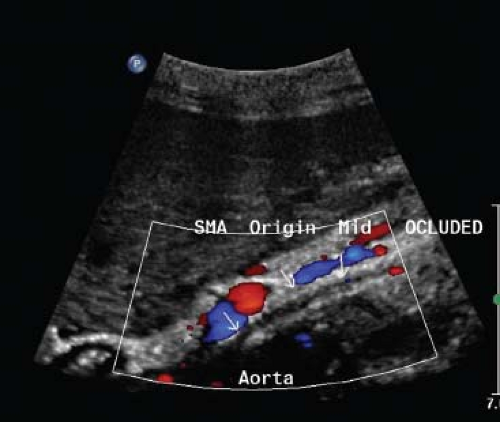
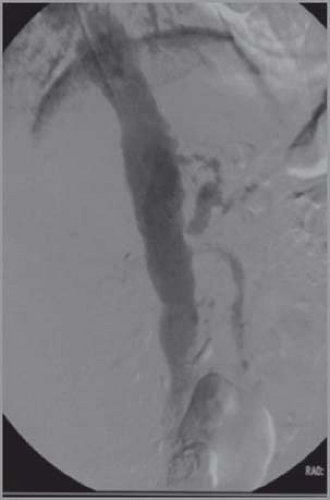
When patients present with symptoms of chronic mesenteric ischemia to the vascular surgeon, they are usually advanced into the disease process. Once the diagnosis is made, prompt revascularization should be undertaken. Many will be malnourished and have persistent symptoms after having undergone cholecystectomy and esophagogastroduodenoscopy. The most common diagnostic screening test is duplex ultrasound (Fig. 11.2), but 64 row slice computerized tomography scans (CT) can provide accurate imaging (Fig. 11.3). All patients undergo aortography and if possible selective angiograms (Fig. 11.4) with attempted percutaneous revascularization. If this is not possible, we move forward with open surgery. We do not generally put the patient through a bowel preparation or preoperative total parenteral nutrition, as they both will overly stress the gastrointestinal tract and liver.
Positioning
Once the decision is made to proceed with visceral aortic endarterectomy, proper positioning will allow the surgeon better intraoperative exposure. Our preference is to use the thoracoretroperitoneal approach as first described by Robb and popularized by Wylie and Stoney. Another option is medial visceral rotation, however this is more time consuming and leads to more third spacing of fluids perioperatively. The patient is placed in the right lateral decubitus position on a bean bag (Fig. 11.5) with the midpoint between the anterior superior iliac spine and the 12th rib, which allows for maximum flexibility. We also no longer use an axillary roll, as this has not been demonstrated to useful. The bed is then flexed and kidney rest elevated. Cushioning is placed at every bony point exposed to pressure, which includes the hips, knees, legs, and back. We pay careful attention to cushioning the legs and place a slight bend in the right leg so as to allow access to check pulses. The Foley catheter is secured underneath the right leg.
Surgical Technique
The case is divided into five steps, each of which carries equal importance to guarantee excellent outcomes.
Opening
Mobilizing the retroperitoneum and taking the spleen down from the diaphragm
Taking down the crus and dissection of the vessels
Endarterectomy
Closing
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree